Filter :
Few outbreaks redefine our perspective on life, and for this generation and the ones to come, the COVID pandemic became a turning point. Years have passed since the pandemic faded from memory, though now another virus is knocking on the nation’s door—the human metapneumovirus (HMPV). However, the question remains: Is it just another seasonal outbreak or a new cause for concern?
HMPV (Human Metapneumovirus) is a single-stranded RNA (Ribonucleic acid) virus that can cause mild to severe illness. HMPV belongs to the Paramyxoviridae family, which is the same family as viruses like Respiratory Syncytial Virus (RSV) and Parainfluenza Virus. HMPV is more prevalent among a few groups of people including,
HMPV can be transmitted by close contact with an infected person or respiratory droplets when an infected person coughs or sneezes or by touching contaminated surfaces and objects and then touching the face, specifically the nose, eyes, and mouth. Individuals infected with HMPV may experience cough, high fever, nasal congestion, sinus blockade, shortness of breath, etc.
Now coming down to the question – Is HMPV just another seasonal outbreak or a new cause of concern?
An experienced doctor sheds light on why HMPV is unlikely to escalate into a pandemic. According to Dr Kuldeep Kumar Grover (CK Birla Hospital) an experienced pulmonologist, HMPV is unlikely to develop into a pandemic. One of the main reasons behind this is that a significant portion of the population already has some level of immunity due to prior exposure to similar viruses. Furthermore, HMPV is regarded as a less potent virus than highly contagious pathogens such as the coronavirus. Its capacity to spread quickly and create widespread outbreaks is significantly less, however, it can cause serious illness in certain groups of people like young children, the elderly, and people with weakened immune systems.
Table of Contents
HMPV spreads through direct contact with bodily fluids or contaminated surfaces and is more likely to spread in crowded places like schools, malls, shopping centers, etc. Listed below are the different ways that the human metapneumovirus spreads.
Spreads when an infected person coughs, sneezes, or talks, tiny droplets carrying the virus travel through the air and can be inhaled by others.
Individuals may contract the virus if they touch a contaminated surface and then touch their face because the virus can survive on surfaces and objects for a short time.
Direct contact with an infected person such as touching, handshake, etc can transmit the virus.
The respiratory virus has recently drawn attention because of its growing prevalence and effects, particularly in the vulnerable group i.e. children, elderly, and those with weakened immune systems. Even though the symptoms are currently mild they could get worse. Among the typical symptoms are the following:
| Mild Symptoms | Severe Symptoms |
| The majority of individuals infected with HMPV have mild symptoms like –
– Cough – Nasal congestion or runny nose – Sinus blockage – Sore throat – High fever – Fatigue |
The cases may progress to severe respiratory issues and cause –
– Shortness of breath or difficulty breathing – Wheezing – Chest tightness – Severe cough – Symptoms of bronchitis – Symptoms of pneumonia |
HMPV can be diagnosed by a pulmonologist through physical examination based on the symptoms and health history. The physical examination involves taking a sample from the nose or throat through a swab.
A lab tests the sample for viruses and other infections. Further, if the symptoms are severe the pulmonologist may recommend certain tests to check for abnormalities:
Early detection and the right treatment of HMPV reduce the risk of severe complications in vulnerable populations.
As of now, there are no antiviral treatments or vaccines available for human metapneumovirus (HMPV). However, the vast majority of reported cases are mild infections that don’t necessitate hospitalisation, though if the symptoms persist for over 3 to 4 days, it is recommended to consult the doctor. Relieving symptoms and aiding the body in its defence against the infection are the main goals of treatment. The key strategies are listed below.
Ensure adequate fluid intake to prevent dehydration, especially during fever or reduced appetite. IV fluids can also be used to maintain hydration and fluids can be directly delivered to your vein (IV).
Use ibuprofen or other medications to treat symptoms like fever or pain and use nasal sprays to clear up congestion in the nose.
Oxygen therapy is recommended for patients who have issues breathing. Oxygen may be provided through a tube in the nose or a mask on your face.
Prescribed medicines and steroids can help reduce inflammation and might ease some of the symptoms.
We can prevent or lower the risk of HMPV in a number of ways including,
What is the HPMV virus?
HMPV (Human Metapneumovirus) is a single-stranded RNA (Ribonucleic acid) virus that can cause mild to severe illness. HMPV belongs to the Paramyxoviridae family, which is the same family as viruses like Respiratory Syncytial Virus (RSV) and Parainfluenza Virus.
What are HMPV virus symptoms?
HMPV can have mild to severe symptoms, mild symptoms include cough, nasal congestion or runny nose, sinus blockage, sore throat, high fever, and fatigue. While severe symptoms include shortness of breath or difficulty breathing, wheezing, chest tightness, severe cough, etc.
Is HMPV in India?
Yes, human metapneumovirus (HMPV) is present in India. However, the number of cases is low.
Brain – The Most Complex Part of the Human Body! Made of complex networks with more than 86 billion neurons, it is responsible for interpreting the senses, initiating body movement, controlling behaviour, and much more. It is a universe in itself, like the vastness of ‘Star Wars’.
A part of the central nervous system, the brain is responsible for controlling thought, emotions, touch, memory, motor skills, vision, breathing, hunger and every process that regulates our body. As you’re reading this blog, your brain is working behind the scenes, processing the words and turning them into meaning. The three-pound organ is the fattiest organ of the human body, comprising 60% fat.
Table of Contents
The analogy of the brain is the same as a computer, the brain takes in information, processes it, and then produces output. The brain comprises several important components like neurons, glial cells, blood vessels, and different regions. One such important part of the brain is the cerebral vein, which is responsible for draining deoxygenated blood away from the cerebrum (the outer part of the brain). The cerebral vein ensures proper blood circulation in the brain.
The more vital an organ is, even a minor issue could lead to serious problems. The same is true for brain-related conditions. One such condition affecting the brain’s function is cerebral venous thrombosis. Defined as a blood clot of a cerebral vein in the brain. Cerebral venous thrombosis is a severe condition that can cause severe headaches, brain swelling, blurred vision, and other life-threatening conditions if not treated appropriately.
The name cerebral venous thrombosis translates to a blood clot in the veins of the brain.
The formation of blood clots affects the normal blood flow in the brain, leading to pressure buildup in the brain. Cerebral venous thrombosis (CVT) can be associated with head injury, infections, certain medications, etc. It is a rare condition, however, if left untreated CVT can lead to a stroke or brain damage.
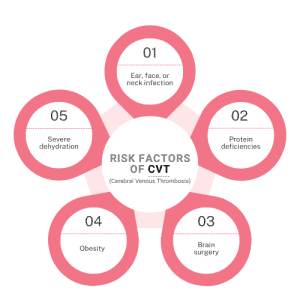
There are various factors that may lead to cerebral venous thrombosis, some of them are listed below:
During pregnancy certain hormones like estrogen, progesterone, etc drastically increase and blood clotting during pregnancy or after delivery may contribute to cerebral venous thrombosis (CVT).
Head injuries occurring out of accidents particularly involving skull fractures damaging brain veins increase the risk of thrombosis.
Various types of infections including, ear infections, sinusitis, meningitis and other infections involving the face or brain can lead to CVT.
Blood clotting tendencies may increase in the body by usage of birth control pills and hormonal therapies.
Conditions like genetic clotting disorder or thrombophilia (a disorder that makes the blood clot more easily) increase the risk of clot formation leading to CVT.
Other less common conditions that may lead to CVT include severe dehydration, certain types of cancer and their treatments, autoimmune diseases, obesity, genetic factors, etc.
According to a research report by ‘The National Center for Biotechnology Information’ (NCBI) cerebral venous thrombosis (CVT) is more common among females. The most common cause of CVT among infants is ear infection. Interruption in regular blood flow may lead to blood clots. However, CVT may be triggered by several factors:
The symptoms of cerebral venous thrombosis can vary depending upon several factors including the location of the clot, severity of blockade, duration, and other individual factors like age, pre-existing medical conditions, etc. Some of the most common symptoms experienced by individuals suffering from cerebral venous thrombosis (CVT) include:
A specialist, usually a neurologist or neurosurgeon can perform a physical examination to evaluate:
The neurologist after comprehending the symptom may suggest certain imaging tests to determine the blood circulation in the brain. Some of the commonly used imaging tests to diagnose CVT are,
Treatment of CVT depends on the severity of the condition. Treatment aims to dissolve clots, prevent them from extending, reestablish proper drainage, manage underlying causes and prevent complications. Treatment of cerebral venous thrombosis involves:
This is usually the first step towards the treatment of CVT. The medicines help prevent blood clots and prevent further clot growth. Some of the commonly prescribed medicines include injectable anticoagulants, oral anticoagulants or blood thinners.
When anticoagulant treatment is ineffective in dissolving the clot, thrombolytics or clot-dissolving treatment is the recommended course of action. Blood clots in blood vessels can be broken by thrombolytics which are medications that are delivered directly to the clots or by breaking the clot using a mechanical device.
This involves the management of symptoms occurring from CVT, such as headaches, pain relievers like acetaminophen or NSAIDs can be used, anti-seizure medications for seizures, etc. Additionally, the brain activity is monitored through follow-up venograms and imaging tests to identify the progress.
| Category | Prevention Strategy |
| Lifestyle | Stay active & hydrated, adopt a healthy diet, quit smoking & manage weight |
| Health Conditions | Manage hypertension, diabetes, clotting disorders & other pre-existing conditions |
| Medications | Use anticoagulants if prescribed & avoid unnecessary hormonal therapy |
| Regular Checkup | Monitor health if at risk or with a specially with a family history of thrombosis |
What is cerebral venous thrombosis?
Cerebral venous thrombosis is a condition causing blood clots of the cerebral vein in the brain. It is a severe condition that can cause headaches, brain swelling, blurred vision, and other life-threatening conditions if not treated appropriately.
Can cerebral venous thrombosis recur?
Yes, cerebral venous thrombosis (CVT) can recur, although the risk is considered low.
Does cerebral venous thrombosis go away?
Yes, cerebral venous thrombosis can go away and be completely cured with prompt diagnosis and treatment.
How is cerebral venous thrombosis treated?
Cerebral venous thrombosis is primarily treated with anticoagulant medications and thrombolytics. For severe cases, surgery may be recommended.
How to diagnose cerebral venous thrombosis?
Diagnosis of CVT can be done through various imaging tests including, Brain MRI, CT Scan, and magnetic resonance venography (MRV).
How to prevent cerebral venous thrombosis?
Prevention of CVT can be done through lifestyle changes, managing underlying medical conditions, adopting a healthy diet, etc.
What are the symptoms of cerebral venous thrombosis?
Some of the common symptoms of CVT are persistent headache, blurred vision, nausea, vomiting, dizziness, balance problems, etc.
We’ve all known for a long time that exposure to toxins harms health, but who would have imagined that the air we breathe could be a slow poison and be one of those toxins?
According to the World Health Organization (WHO), air pollution kills an estimated seven million people worldwide yearly. Air pollution is the contamination of air by substances that are harmful to humans or other living beings and damage the environment.
Breathing polluted air is known to impact almost every organ in the body. Most commonly air pollution affects the respiratory tract, it is the main pathway of exposure to air pollution and can lead to issues like asthma, bronchitis, etc. Recent studies also indicate that exposure to particulate matter (PM 2.5, PM 10) and nitrogen dioxide (NO2) are leading contributors to the rising number of health conditions like respiratory issues, cardiovascular problems, renal conditions, and even cancer. According to a recent report by ‘The Hindu’ lung cancer cases are increasing in non-smokers and air pollution is believed to be the culprit.
An expert pulmonologist at the CK Birla Hospital, Dr. Kuldeep Kumar Grover asserts that lung infections and air quality are directly related. You run a greater risk of getting respiratory ailments the more polluted the air you breathe. Asthma, bronchitis, COPD, lung cancer, and other lung conditions are caused by high levels of pollutants, especially PM2. 5 which are small enough to penetrate deep into the lungs. Reducing exposure to air pollution is the only way to ensure your safety. Additionally, avoiding eating outside food can help minimise the risk of aerophagia (swallowing of air).
Table of Contents
The lungs are an important organ that helps us breathe. The primary role of the lungs is to absorb oxygen from the air we breathe and remove carbon dioxide. Additionally, the lungs help break down blood clots, regulate blood pressure, maintain the body’s acid level balance, support the sense of smell, etc. The main organ of the respiratory system is located in the chest cavity.
A number of illnesses can interfere with the lung’s normal function resulting in symptoms like shortness of breath, sleeplessness, irregular breathing, loss of consciousness, restlessness, and other related issues. Lung disorders are primarily caused by infections, environmental factors, or abnormal cell growth. One such potentially severe life-threatening condition is lung cancer.
According to a recent report, lung cancer is a common cancer and a leading cause of cancer-related death in India. A leading contributing factor to this rising number is the usage of tobacco smoking. The spread of cancer is further categorized into stages, including
Lung cancer usually starts in the airways or small air sacs. Various types of cancer affect the lungs, however, there are two main types of lung cancer.
The last several decades have seen a major global concern over air pollution. A wide range of diseases can result from both short-term and long-term exposure to pollutants and the majority of people live in areas where pollution levels can rise. One of the main causes of cancer according to the International Agency for Research on Cancer (IARC) is air pollution, specifically PM 2.5. Additionally, chronic exposure can impact all of the body’s organs complicating and aggravating pre-existing medical conditions. Air pollution can cause a variety of health problems:
Pollutants present in the air we breathe can increase the risk of respiratory infections like pneumonia.
Pollutants like PM2.5 and nitrogen dioxide can enter the bloodstream and increase the risk of heart attacks, high blood pressure, etc.
Pollutants can penetrate deep into the lungs, causing inflammation, DNA damage, and oxidative stress leading to cancer.
Exposure to harmful pollutants irritates and inflames the airways leading to damage of lung tissues & reducing lung function and other related conditions.
Long-term exposure to pollutants can result in weakening of the immune response making individuals more susceptible to infections.
Long-term exposure to substances like benzene, polycyclic aromatic hydrocarbons, and PM2.5 increases the risk of developing bladder cancer, breast cancer, Leukemia, and other types of cancer.
Despite the fact that tobacco products and cigarette packets are marked as they cause cancer a sizable section of the populace still consumes them. Tobacco remains the leading cause of the growing number of lung cancer cases. Air pollution has also been identified as an emerging factor. Even though there are fewer cases connected to air pollution the tendency to overlook such issues in their early stages persists. It’s crucial to address this perspective and act proactively.
Exposure to pollutants like PM2.5, nitrogen dioxide, polycyclic aromatic hydrocarbons, etc penetrate deep into the lungs causing,
Leading to mutation and cancer cell growth. Additionally, prolonged exposure to such pollutants disrupts the cell repair mechanism and weakens the immune system, increasing the risk of cancer over time. Other lung issues caused by air pollution include,
Difficulty breathing or feeling out of breath with routine activities is a clear symptom of lung damage due to air pollution.
Individuals experience congestion or discomfort in the chest region due to exposure to harmful pollutants.
A common sign indicating poor air quality is impacting the lungs is excessive phlegm or mucus production as the lungs try to clear irritants & pollutants.
Dryness or soreness may be felt in the pharynx due to long-term or even short-term exposure to pollutants.
Individuals may experience whistling or squeaky sounds while breathing indicating airway constriction.
Respiratory Infections like recurring colds, bronchitis, or pneumonia may be experienced by individuals indicating lung damage
During the developing phase or growing phase the lungs are more sensitive to pollutants. Additionally, children are more active and breathe faster, increasing the level of exposure.
With age lung function naturally weakens and the immunity level declines making the elderly population more prone to such lung conditions.
Exposure to pollutants affects maternal lung health and can increase the risk of adverse pregnancy outcomes, like preterm birth, low birth weight, etc.
Individuals already diagnosed with asthma, COPD, or bronchitis are at higher risk of exacerbations.
Air pollution is known to worsen cardiovascular health, leading to individuals with various heart conditions at high risk.
Smoking affects normal lung function, leaving smokers and former smokers with damaged lungs more vulnerable to health risks due to exposure to pollutants.
People living in urban areas are more exposed to pollutants from traffic emissions, industrial pollutants, etc increasing the risk.
The risk of developing lung-related conditions can be raised by exposure to harmful substances and certain environmental factors. Key risk factors include:
| Factors | Preventive Measures |
| Smoking | Quit smoking & avoid secondhand smoke exposure |
| Air Pollution | Wear masks, use air purifiers & limit staying outdoors during high-pollution |
| Indoor Air Pollution | Ensure proper ventilation & avoid using solid fuels |
| Infections | Get vaccinated (e.g, flu, pneumonia) & practice good hygiene. |
| Allergens | Do regular cleaning & use air filters to reduce exposure |
| Chemical Exposure | Use eco-friendly products & avoid contact & inhaling of harsh chemicals |
Is lung cancer curable?
Lung cancer is not usually curable, however, some cases may be cured if diagnosed before they spread. The outlook depends on the stage of the cancer, age, and overall health.
What are the symptoms of lung cancer?
Some of the common symptoms of lung cancer include coughing, shortness of breath, wheezing, chest pain, blood clots, etc.
How is lung cancer detected?
Lung cancer is detected through imaging tests like chest x-ray, CT scan, MRI, PET scan and tissue samples like sputum test, core biopsy, etc.
Can lung cancer be detected by x-ray?
Yes, lung cancer can be detected by chest x-rays.
What causes lung cancer?
Lung cancer may be caused by several factors including, smoking, exposure to certain chemicals, exposure to pollutants like PM 2.5, etc.
Can lung cancer be cured at stage 4?
No, stage 4 lung cancer is not curable, but it can be treated, the treatment goal focuses on relieving symptoms, improving quality of life, and prolonging life.
Is lung cancer genetic?
Yes, lung cancer can be genetic.
Table of Contents
Winter is the best time of the year when it comes to nature’s bounty of nutrients. Nuts like almonds, although now available round the year, are often associated with the best winter delicacies and bakes. Cherished by all for its crunch, flavor, and outstanding nutritional value, almond is highly versatile as a nutrient rich snack in winters. From smoothies to salads, almonds can help speed up your fat-to-fit journey effectively.
But the question arises—should you eat them raw, or soaked? The answer? Soaked almonds reign supreme. Not only do they improve digestion, but they also unlock a greater nutritional profile, essential for those who are plagued by weight fluctuations. Let us understand why soaking almonds could be the ultimate game-changer for your fitness goals.
These beautiful nuts are packed with fiber, protein, and healthy omega fats. But despite being a complete power food, almonds are protected by a tannin rich brown skin. Therefore, soaking almonds overnight helps remove this skin, making the nutrients more bioavailable and easier to digest. Here is a list of benefits of soaking almonds:
Superfood Myth: Only Raw Almonds Are NutritiousFact: Soaked almonds are easier to digest and absorb, making them a superior option compared to raw almonds. |
Soaked almonds aren’t just a delicious snack; they are a powerhouse for those looking to shed extra pounds. Here’s how:
Fiber and protein content in almonds can curb hunger cravings. Soaked almonds in the morning can curb the tendencies of excessive snacking throughout the day. This directly makes calorie tracking easier.
It has been proven that the presence of magnesium in almonds helps regulate metabolism. A faster metabolism helps burn more calories efficiently, supporting weight loss.
Consuming healthy fats can help lose weight without gaining it. The monounsaturated fats omega fatty acids in almonds reduce unhealthy cravings and prevent overeating, helping you maintain a balanced diet.
Soaked almonds promote good bacteria in the gut, improving digestion and reducing bloating. This is one of the most important factors in your weight loss journey as you gain healthy and natural outcomes without any intervention of supplements.
Studies suggest that almonds help in lowering LDL (bad cholesterol) while increasing HDL (good cholesterol). This is important for your cardiac wellness as a better lipid profile is the direct outcome of better weight management.
An erratic blood sugar spike can be the reason for frequent hunger pangs and overeating. The low GI (glycemic index) of almonds stabilize blood sugar levels, preventing sudden spikes and crashes.
Superfood Myth: Eating Too Many Almonds Can Make You FatFact: Portion control is key. Consuming around 6-10 almonds per day is ideal for weight loss without excessive calorie intake. |
To get the maximum benefit from almonds, it’s essential to soak them correctly. Here’s a simple step-by-step guide:

Pro Tip: If you forget to soak almonds overnight, soak them in hot water for 30 minutes to achieve similar benefits.
Superfood Myth: Almonds Are High Calorie, So They Are Bad for Weight LossFact: While almonds are calorie-dense, they have a high satiety index, meaning they keep you full for longer, preventing overeating. |
Also Read: Healthy Diet Chart for High Blood Pressure Patients
From boosting metabolism and curbing hunger to improving digestion and stabilizing blood sugar, these nutrient-dense nuts offer a holistic approach to better health.
If you’re looking for a simple and natural way towards weight loss, start soaking almonds today! Small habits like these can make a big difference in long-term health and wellness.
So, are you ready to unlock the power of soaked almonds and transform your weight loss game? Start today and enjoy the benefits of this superfood!
FAQs
How many soaked almonds should I eat daily for weight loss?
A handful (6-10 almonds) per day is enough. Using almonds you can sufficiently gain benefits without excessive calorie intake.
Can I drink the water used for soaking almonds?
The whole purpose of soaking almonds is to eliminate the tannins from its brown cover. It is best to discard the soaking water, in order to eliminate enzyme inhibitors from the almonds.
Can I eat soaked almonds at night?
Yes! While morning consumption is ideal, eating soaked almonds at night can also be beneficial for digestion and metabolism.
Are roasted almonds good for weight loss?
While roasted almonds are tasty, they may contain added oils and salt. Soaked almonds are the best option for optimal health benefits.
Do soaked almonds improve skin and hair health? Absolutely! The vitamin E and antioxidants in almonds nourish the skin and promote hair growth, making them a beauty-enhancing superfood as well.
Over time cancer cases in women have been notably on the rise. Cervical Cancer after Breast Cancer is affecting Indian women the most. Recent data from MediAssist Healthcare Services reveals that cancer-related insurance claims surged in 2024, with a significant rise among women aged 40 and above.* Cervical cancer remains a leading cause of cancer-related deaths among women in the country. It’s a wake-up call, especially for women in India who need to know ways to prevent cervical cancer and stay protected.
** Source: The Lancet
The good news is that Cervical Cancer is preventable, as it is the only cancer with a vaccine. And so being proactive against the HPV virus that causes cervical cancer can be the best approach. This Cervical Cancer Awareness Month, let’s understand how the HPV vaccine can make a difference.
Table of Contents
Cervical cancer is usually the outcome of an HPV infection. HPV is a group of viruses, with over 100 strains and can be transmitted through sexual contact. Most HPV infections clear naturally, some however overstay their welcome, leading to abnormal cervical cell growth and, eventually, cancer. Studies suggest that predominantly strain types 16 and 18 are responsible for causing about 70% of all recorded cervical cancer cases.
But Cervical Cancer cells need certain contributing factors in order to manifest and evolve.
If someone is already experiencing conditions like HIV or are under long-term steroid use due to other diseases, then they are certainly more susceptible to develop cancer. A weak immune system is the perfect base to manifest cancer cells.
Today smoking is prevalent in men and women alike and is therefore the most common contributor to causing cancer. The oxidation process of smoking has been proven to harm cervical cells and therefore impair immunity. This poor lifestyle choice is affecting more and more people everyday.
The cervical region needs extra attention as poor hygiene practices can lead to heightened infection risks. This means proper usage of clean sanitary napkins, regular cleaning and special care during menstruation among women. This also applies to keeping the region clean post sexual activity.
Prolonged use may slightly increase cancer risk. Many women are prescribed contraceptives to treat various other problems, such as hormonal imbalance, irregular periods and PCOS. It is very important to discuss this with your doctor to ensure one problem does not invite another.
HPV is sexually transmitted. Therefore a vast majority of sexually active individuals will contract HPV at some point of time in their lives. This makes vaccination and screening essential.
The HPV vaccine protects against the most common cancer-causing strains of HPV (types 16 and 18), reducing the risk of cervical, vaginal, and vulvar cancers.
Answer these questions to assess your risk:
If you got more than two Yes-s, it is time you visited your doctor.
Think of a Pap smear as your cervical health’s early warning system. This quick and straightforward test is like a radar, spotting abnormal cell changes long before they turn into something more serious, like cervical cancer.
For women aged 21 and above, regular Pap smears aren’t just a recommendation—they’re a lifesaver. Pair it with the HPV vaccine, and you’ve got a one-two punch against cervical cancer. Remember, prevention is always better than cure.
If any of these apply to you, consult a healthcare provider for a Pap smear or HPV test. Early detection saves lives.
Cancer cannot be cured, but it can be prevented. Cervical cancer is the only cancer that comes with a vaccine. Then grab this time sensitive opportunity to stay one step ahead, proactively. Consult your doctor about eligibility and timing.
Early detection is the best approach to cancer. If you have exceeded the age bracket for the vaccine, then pap smears are your best alternative. Pap smears are effective as they detect precancerous changes early, making it easier to prevent things from going out of hand. But one must be regular with this and discuss a screening schedule with their gynaecologist.
Choosing a good lifestyle and consistently ensuring proper menstrual hygiene can prevent any kind of gynaecological anomalies from affecting your life. Eat healthy and quit smoking to buy yourself time away from a host of life altering diseases.
“As a doctor, I’ve seen the toll cervical cancer takes on women and families,” says Dr. Aruna Kalra, Consultant Gynecologist at the CK Birla Hospital. “The HPV vaccine is one of the most effective tools we have to protect against this preventable disease. Vaccination combined with regular screenings is your best bet for safeguarding your health.”
Cervical cancer is preventable. This Cervical Cancer Awareness Month, prioritise your health by learning about the HPV vaccine and encouraging others to do the same. Awareness and early action can save lives.
Share this with your loved ones and take the first step toward a healthier future. For more information, contact us at https://www.ckbhospital.com/doctors/cervical-cancer-treatment-doctors-in-delhi/
क्या आपका सिर भी हमेशा भारी रहता है? सिर में भारीपन के कारण दर्द होता है जो आपके दैनिक जीवन को बुरी तरह प्रभावित करता है? अगर हाँ, तो यह ब्लॉग आपके लिए है। इसमें हम सिर में भारीपन के कारण, मेडिकल उपचार और घरेलू उपायों के बारे में बात करेंगे।
Table of Contents
नींद की कमी, लो ब्लड प्रेशर (निम्न रक्तचाप), साइनसाइटिस (साइनस का संक्रमण), डिहाइड्रेशन (शरीर में पानी की कमी), आँखों की समस्या, तनाव, कान का दर्द या या कान की समस्या, मोशन सिकनेस, दवाओं का प्रभाव और पैनिक अटैक
हाइड्रेटेड रहें, पश्चिमोत्तानासन योग करें, धनिया और चीनी का घोल, अदरक का पेस्ट माथे पर लगा सकते हैं, चंदन का पेस्ट माथे पर लगा सकते हैं, नींबू पानी पीएं, लौंग और दूध का पेस्ट सेवन कर सकते हैं, दूध और बादाम का सेवन कर सकते हैं संतुलित आहार लें और पर्याप्त नींद लें
नियमित स्ट्रेचिंग और व्यायाम करें, धूम्रपान और शराब से बचें, स्वस्थ आहार का सेवन करें
ये भी पढ़े: कमर दर्द क्यों होता है — कारण और घरेलू इलाज (Back Pain in Hindi)
सिर में भारीपन कई वजहों से हो सकता है। हालांकि, इसके सामान्य कारणों में निम्न शामिल हो सकते हैं:
इन सबके अलावा, अन्य भी अनेक न्यूरोलॉजिकल कारण हैं जिससे सिर में भारीपन की समस्या पैदा हो सकती है।
ये भी पढ़े: जोड़ों में दर्द का कारण, लक्षण और उपचार | Joint pain in hindi
सिर में भारीपन का उपचार कई तरह से किया जाता है। कुछ विशेष जांच की मदद से डॉक्टर सिर में भारीपन के सटीक कारण का पता लगाते हैं। उसके बाद, सिर में दर्द के कारण (sir me dard ke karan), मरीज की उम्र, उसका सम्पूर्ण स्वास्थ्य और पहले से मौजूद बीमारियों को ध्यान में रखते हुए उपचार की योजना बनाते हैं। मेडिकल उपचार के साथ-साथ मरीज को जीवनशैली में बदलाव लाने का भी सुझाव दिया जाता है।
ये भी पढ़े: नसों में दर्द का कारण और उपचार | Nerve Pain in Hindi
सिर में भारीपन से राहत पाने के लिए आप डॉक्टर से परामर्श करने के बाद निचे दिए गए उपायों को आजमा सकते हैं:
इन सबके अलावा, नियमित रूप से स्ट्रेचिंग करें और धूम्रपान एवं शराब आदि से बचें। अगर आपके सिर में भारीपन रहता है और घरेलू नुस्खों को अपनाने के बाद भी कोई लाभ नहीं हुआ तो डॉक्टर से बात करके उचित जांच और उपचार पर विचार करें।
अगर लगातार आपके सिर में भारीपन महसूस हो रहा है, तो तुरंत डॉक्टर से संपर्क करना चाहिए। सिर में भारीपन की समस्या कई कारणों से हो सकती है, जैसे कि सिरदर्द, साइनस संक्रमण, ब्रेन ट्यूमर या कोई न्यूरोलॉजिकल डिसऑर्डर आदि। अधिकतर मामलों में, सिर भारी लगने की समस्या गंभीर नहीं होती है।
अगर आपको सिर में भारीपन के कारण सिर में गंभीर दर्द है या आपका सिरदर्द गंभीर हो रहा है, तो आपको तुरंत डॉक्टर से परामर्श लेना चाहिए। साथ ही, अगर आपको नीचे दिए गए लक्षणों का अनुभव करते हैं तो इमरजेंसी मेडिकल सहायता लेनी चाहिए:
साथ ही, अगर आपको खड़े होने पर बार-बार या लगातार चक्कर आते हैं तो आपको डॉक्टर को दिखाना चाहिए।
काला पीलिया एक गंभीर समस्या है जिसके लक्षणों पर ध्यान देना और समय पर डॉक्टर से परामर्श करके उचित उपचार पाना आवश्यक है। इस ब्लॉग में हम काला पीलिया के कारण, लक्षण और उपचार के बारे में विस्तार से जानेंगे।
Table of Contents
लिवर में होने वाला एक घातक वायरल इंफेक्शन है काला पीलिया, जो हेपेटाइटिस बी और सी वायरस के संक्रमण की वजह से होता है। जब लिवर में हेपेटाइटिस का इंफेक्शन बहुत ज्यादा बढ़ जाता है, तब लिवर सिरोसिस और लिवर कैंसर की स्थिति पैदा हो जाती है। ऐसी स्थिति में मरीज की मौत भी हो सकती है। काला पीलिया, बॉडी फ्लूइड से एक व्यक्ति से दूसरे व्यक्ति में फैल सकता है।
ये भी पढ़े: थायराइड क्या है – कारण, लक्षण और घरेलू उपचार (Home Remedies For Thyroid in Hindi)
आमतौर पर काला पीलिया के लक्षण सामान्य पीलिया के जैसे ही होते हैं, लेकिन कुछ मामलों में यह भिन्न हो सकते हैं। काला पीलिया होने के बाद मरीज खुद में लक्षणों का अनुभव कर सकते हैं जैसे कि:
काला पीलिया एक गंभीर लिवर की बीमारी है जिससे लिवर को नुकसान पहुंचता है। अगर समय पर इलाज न किया जाए, तो लिवर में कार्बन जमा हो सकता है, जिससे कैंसर, किडनी को नुकसान और त्वचा से जुड़ी परेशानियां पैदा हो सकती हैं। इसलिए अगर आप खुद में ऊपर दिए गए लक्षणों का अनुभव करते हैं या आपको इस बात की आशंका है कि आपको काला पीलिया है तो बिना देरी किए डॉक्टर से मिलें।
ये भी पढ़े: गाइनेकोमैस्टिया क्या है – कारण, लक्षण और उपचार (Gynecomastia in Hindi)
काला पीलिया होने पर शरीर में बिलीरुबिन का स्तर बढ़ जाता है, जिससे त्वचा और आंखों का सफेद हिस्सा पीला पड़ जाता है। काला पीलिया को आम बोलचाल में ब्लैक जॉन्डिस भी कहते हैं। इसके कुछ कारण हैं जैसे कि:
ऊपर दिए गए कारणों को ध्यान में रखकर इस बीमारी से खुद को बचाया जा सकता है।
ये भी पढ़े: क्या सामान्य ज़ुकाम, खांसी या ठंड निमोनिया में बदल सकती है
काला पीलिया की जांच के लिए, डॉक्टर बिलीरुबिन परीक्षण करवाने की सलाह देते हैं। इस परीक्षण में, रक्त के तरल भाग यानी सीरम में बिलीरुबिन का स्तर मापा जाता है। अगर बिलीरुबिन का स्तर सामान्य से 2-3 गुना ज्यादा है, तो पीलिया के लक्षण हो सकते हैं।
काला पीलिया का निदान करने के लिए डॉक्टर कुछ जांच करने का सुझाव देते हैं, जिनमें निम्न शामिल हैं:
अन्य टेस्ट जो किए जा सकते हैं उनमें शामिल हैं हेपेटाइटिस वायरस पैनल, कोलेस्ट्रॉल लेवल और प्रोथ्रोम्बिन समय आदि।
काला पीलिया में तत्काल मेडिकल देखभाल और अस्पताल में भर्ती होने की आवश्यकता होती है। उपचार के विकल्पों में निम्न शामिल हैं:
काला पीलिया के अन्य उपचारों में दलिया के साथ गर्म स्नान, एंटीहिस्टामिन, कोलेस्टारामिन या कोलस्टिपोल, लिवर ट्रांसप्लांट, ब्लॉक बाइल डक्ट को खोलने के लिए सर्जरी, फोटोथेरेपी – जो बिलीरुबिन को तोड़ने के लिए फ्लोरोसेंट रोशनी का उपयोग करती है आदि शामिल हो सकते हैं।
काले पीलिया से बचने के लिए आप कुछ नीचे दिए गए उपायों को अपनाए जा सकते हैं:
पीलिया से जल्दी निजात पाने या उससे बचने के लिए ये घरेलू उपाय अपनाए जा सकते हैं। अगर इसके बारे में विस्तार से जानना चाहते हैं तो डॉक्टर से बात करें।
फेफड़ों में कई तरह की बीमारियों होती हैं, पल्मोनरी एडिमा यानी फेफड़ों में पानी भरना भी उन्हीं में से एक है। इस स्थिति में फेफड़ों में मौजूद छोटी-छोटी थैलियों में पानी या द्रव जमा हो जाता है जिसके कारण मरीज को सांस में लेने में कठिनाई होती है।
Table of Contents
फेफड़ों में पानी भरना एक गंभीर समस्या हो सकती है जिसका समय पर जांच और उपचार आवश्यक है। फेफड़ों में पानी या तरल पदार्थ जमा होने पर शरीर में ऑक्सीजन की कमी होती है। साथ ही, दिल की मांसपेशियां खून को पम्प करने में असमर्थ होती हैं, जिससे दिल को अधिक मेहनत करनी पड़ती है। ऐसी स्थिति में ब्लड वैसेल्स पर एक्स्ट्रा प्रेशर पड़ता है और फेफड़े पर्याप्त मात्रा में हवा नहीं ले पाते हैं और मरीज को सांस लेने में दिक्कत होती है।
फेफड़ों में पानी जमा होने के अनेक कारण हो सकते हैं। आमतौर पर निमोनिया होने या शरीर का कोई अंग खराब होने पर (जैसे कि हार्ट फेल्योर, किडनी खराब होना या लिवर सिरोसिस आदि) फेफड़ों में पानी भरने लगता है। इन सबके अलावा, निम्न स्वास्थ्य समस्याएं इसका कारण बन सकती हैं:
साथ ही, धमनियों (आर्टरीज) के सिकुड़ने पर भी फेफड़ों में पानी जमा होने का खतरा बढ़ जाता है।
फेफड़ों में पानी जमा होने पर डॉक्टर कुछ परीक्षण करने का सुझाव देते हैं जैसे कि:
फेफड़ों में तरल पदार्थ का पता लगाने के लिए छाती का एक्स-रे कराया जाता है। यह आमतौर पर सबसे पहला परीक्षण होता है।
फेफड़ों में पानी भरने की जांच के लिए अल्ट्रासाउंड भी कराया जा सकता है। जब एक्स-रे से कुछ चीजों की पुष्टि नहीं हो पाती है तो अल्ट्रासाउंड किया जाता है।
ब्लड टेस्ट से अंतर्निहित कारण का पता लगाने में मदद मिलती है। इसमें ब्लड का सैंपल लेकर लैब में जांच के लिए भेजा जाता है।
यह परीक्षण दिल की इमेज बनाने के लिए ध्वनि तरंगों का इस्तेमाल करता है। इससे दिल से जुड़े कारणों का पता चलता है।
फेफड़ों में जमा पानी या तरल पदार्थ को निकालने के लिए थोरासेंटेसिस प्रक्रिया की जाती है। इसमें, दो निचली पसलियों के बीच की त्वचा में एनेस्थीसिया दिया जाता है और फिर एक छोटी सी सुई डाली जाती है। पानी को निकालने के बाद, फेफड़ों में पानी और मवाद बनने की वजह का पता लगाया जा सकता है।
फेफड़ों में पानी भरने के कारण मरीज को सांस लेने में परेशानी होने लगती है। इसलिए इस बीमारी का जल्द से जल्द इलाज करना आवश्यक होता है। मरीज के शरीर में ऑक्सीजन की पूर्ति करना इस बीमारी के इलाज में सबसे पहला कदम होता है। मरीज को प्रॉपर ऑक्सीजन मिल सके इसलिए ऑक्सीजन मास्क या अन्य उपकरण का इस्तेमाल किया जाता है।
उसके बाद, फेफड़ों में पानी जमा होने के सटीक कारण का पता लगाकर, उपचार योजना बनाई जाती है। आमतौर पर उपचार के तौर पर कुछ दवाएं निर्धारित की जाती हैं जो फेफड़ों से एक्स्ट्रा पानी को निकालने, दिल की मांसपेशियों को मजबूत बनाने और धड़कनों को कंट्रोल करने का काम करती हैं।
कई बार जब दवाओं से कोई फायदा नहीं होता है या मरीज की स्थिति गंभीर होती है तो उसे आईसीयू (इंटेंसिव केयर यूनिट) में एडमिट किया जा सकता है। इन सबके अलावा, मरीज को अपनी लाइफस्टाइल और खानपान में कुछ ख़ास बदलाव करने का भी सुझाव दिया जाता है।
फेफड़ों में पानी भरने पर जल्द से जल्द उपचार पाना आवश्यक है, क्योंकि उपचार में देरी होने पर ऑक्सीजन की कमी के कारण मरीज की मृत्यु भी हो सकती है। समय पर सही उपचार से फेफड़ों में जमा पानी बाहर निकालने के कुछ ही दिनों के अंदर मरीज ठीक हो जाते हैं। हालाँकि, कुछ मरीजों को लंबे समय तक ब्रीडिंग मशीन (सांस लेने में मदद करने वाली मशीन) का इस्तेमाल करना पड़ सकता है।
Polycystic Ovary Disease (PCOD) is a medical condition diagnosed in females during the reproductive age. The condition causes the ovaries to produce more immature or partially mature eggs which accumulate in the ovary. Over time these immature or partially mature eggs begin to develop into cysts which cause the release of excess amounts of androgens, a hormone leading to irregular periods, infertility, and other health problems.
According to Unicef.org, about one-third of menstruating women around the world suffer from PCOD. Lifestyle factors like chronic stress, an unhealthy diet, and an inactive lifestyle can be linked to this enormous number. Females suffering from PCOD can experience issues like heavy bleeding during periods, irregular menstrual periods, sleep disorders, depression, difficulty getting pregnant, skin darkening, etc.
Table of Contents
The exact cause of PCOD is still unknown, though several factors influence the hormone level and ovarian function leading to PCOD including,
Insulin produced by the pancreas helps regulate the blood sugar level in the body. The excess insulin level leads to the overproduction of androgens affecting ovulation.
Several studies reveal indicators connected to genetic sequences associated with PCOD. Individuals may be at greater risk if a close family member has it.
Unhealthy lifestyle habits like excessive consumption of junk food, heavy smoking and alcohol consumption may also cause conditions like PCOD and other related disorders.
A hormonal imbalance and insulin resistance caused by obesity can also result in PCOD.
Low-grade inflammation due to various reasons can trigger the ovaries to overproduce androgens contributing to PCOD.
Keeping up a healthy diet is beneficial for overall health, particularly for people facing PCOD and related conditions. If a customised diet plan is followed while managing PCOD it can help with weight control, insulin sensitivity, support hormonal imbalance, and reduce inflammation. A combined approach involving regular exercising, stress management, and making healthy dietary changes can help with the effective management of PCOD. The recommended food that helps with managing PCOD includes,
Insulin resistance is frequently linked to polycystic ovarian disease. Including foods high in fibre in your daily diet can help keep the blood sugar levels stable. The diet should include vegetables that are high in fibre such as spinach, broccoli, etc.
Consuming healthy fats helps with hormone production, lowers inflammation, and promotes hormone imbalance. Including products with healthy fats like avocados, nuts, flax seeds, chia seeds, etc in daily diet can help effectively manage PCOD and other related conditions.
Adding protein to the daily diet like fish, tofu, lentils, etc. can help support muscle health, promote a feeling of fullness, and help regulate hormones.
Foods that are high in antioxidants can help control stress, lower inflammation, and balance insulin production. Berries, spinach, avocado, nuts, olive oil and, other foods can all help increase antioxidant levels managing PCOD effectively.
Green teas and spearmint tea are rich in antioxidants and are known to have anti-androgen properties. Including these in your regular diet can help with improving insulin sensitivity.
Additional foods and products to incorporate into the daily diet to manage PCOD include fruits and vegetables with a low glycemic index (GI), omega-3-rich foods, fermented foods, green leafy vegetables, etc.
Some foods can help maintain hormonal balance while others can worsen hormonal imbalance, increase inflammation, and aggravate insulin resistance. Certain food categories can exacerbate the symptoms of PCOD and should be avoided including:
| Category | Examples |
| Refined Carbohydrates | White bread, white rice, pasta, cookies, muffins |
| Processed & Junk Foods | Chips, fast food, frozen meals, packaged snacks |
| Sugary Beverages | Sodas, sweetened coffee/tea, energy drinks, fruit juices |
| Alcohol | Beer, wine, spirits, cocktails |
| Red & Processed Meats | Bacon, sausages, salami, fatty red meats |
A balanced diet for managing PCOD promotes balancing hormones, reducing inflammation, managing insulin resistance, and maintaining a healthy weight. Since, PCOD is a chronic condition and can’t be cured, following a balanced diet and avoiding the triggering food & products can help manage the symptoms and reduce the risk of long-term complications and promote the overall quality of life. Under the direction of a nutritionist or specialist a customised diet plan is created with the patient’s overall health in mind. It aids in the efficient management of the symptoms related to PCOD and fosters long-term health.
What are the complications of the PCOD problem?
There are various complications related to PCOD, including infertility, depression, obesity, sleep apnea, etc. Changes in lifestyle, medication, supervision, etc. can all help manage these complications.
Why does PCOD cause weight gain?
PCOD is a condition when excessive hormones called androgens are produced. Elevated androgen levels can increase appetite, and promote abdominal fat storage leading to weight gain.
When is PCOD dangerous?
PCOD can have serious consequences including an increased risk of diabetes, heart disease, pregnancy complications, and other illnesses if left untreated/unmanaged.