Personal hygiene is a crucial part of staying healthy. Excess humidity, a warm climate, and lack of personal hygiene are enhancing factors of UTIs (urinary tract infections), which include Chlamydia trachomatis.
However, unlike yeast overgrowth or fungal infections, the transmission of chlamydia happens through sexual contact.
Chlamydia is a silent spreader because there are no visible symptoms during its incubation period (lasting between a few weeks to six months). Besides, individuals having active and unprotected sex life are most vulnerable to contracting it.
Table of Contents
Named after its causative agent, Chlamydia trachomatis, chlamydia is a bacterial infection that affects the reproductive tract in both genders.
Chlamydia is the most prevalent STI, spreading rapidly often without the knowledge of the carrier, given the dormant character of the bacterium.
This condition can stay undetected until intense physical discomfort (pain during intimacy, difficulty in passing urine, or pelvic pain) post-incubation. Besides, chlamydia isn’t incurable like HIV. Seeking prompt treatment can cure this bacteria-borne STI.
Chlamydia infection spreads through sexual contact (both oral and penetrative). It can also infect a healthy individual using sex toys or indulging in self-pleasure with a silent carrier. Prevalent pathways include:
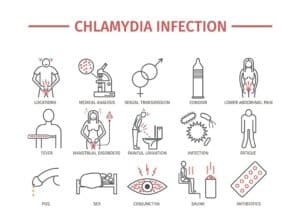
We understand the stigma associated with STI patients, especially since most are incurable. While chlamydia is curable, some things that don’t lead to the spreading of the bacteria are as follows:
Chlamydia affects irrespective of gender, making both men and women silent carriers.
Symptoms displayed are different for both genders. It’s difficult to self-diagnose because they resemble PID (pelvic inflammatory disease) and cervical issues (cervicitis).
Here’s what chlamydia in men and women looks like:
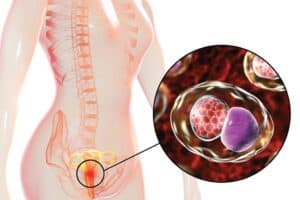
Chlamydia is a UTI (urinary tract infection). It can affect the urogenital tract, secreting discharge from the penis. The following symptoms suggest chlamydia in men:
Besides, most men often report being asymptomatic for a long time. If you are having oral sex with a suspected Chlamydia trachomatis patient, you might develop throat issues rather than contamination around the urinogenital tract.
Chlamydia infection in women often stays hidden, devoid of symptoms immediately after contracting this STI. Prevalent symptoms show similarities with ovarian problems like PCOS and ovarian torsion, worsening the issue if the patient attempts to self-diagnose.
Here’s what to look for in chlamydia among women:
Women are prone to be silent carriers of chlamydia infection. It can also infect the rectum (anal penetration) and throat (oral sex), making it deadly enough to affect various parts of your body at once.
Contracting chlamydia requires:
Chlamydia trachomatis can only spread through sexual contact between a healthy person and a potential silent carrier. People at risk of contracting it include:
Here are the risks associated with having chlamydia in men:
While chlamydia in women has serious side effects for both the mother and her unborn baby, complications include:
Chlamydia is a curable illness. Although chlamydia prevention is the best choice, antibiotics are the preferred treatment (since chlamydia trachomatis is a bacterium).
Your physician may prescribe you the following antibiotics:
Besides treatment, preventive behavior is the best course for chlamydia prevention. It includes:
Before making an appointment with your physician, know the chlamydia symptoms well or look for its gender-based side effects. You should make an immediate appointment if you are:
It’s crucial to maintain sexual distinction to prevent the spread of chlamydia infection. Never hesitate to reach out to your physician if you show suspected symptoms similar to chlamydia.
Not sure where to discuss your chlamydia symptoms with privacy? Visit the CK Birla Hospital near you or book an appointment with Dr. Astha Dayal to learn more about chlamydia treatment.
Q1. Is chlamydia a serious STD?
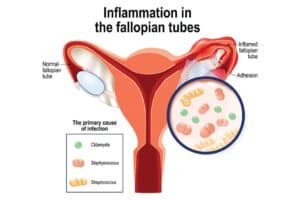
Chlamydia is a curable STD, making it not a severe condition, unlike HIV. However, if left untreated, it worsens to affect both the testis (reducing fertility) and fallopian tubes (risking ectopic pregnancy).
Q2. How do I know if I have chlamydia?/How to know if you have chlamydia?
Chlamydia symptoms, like a burning sensation during urination or smelly discharge from the urethra/vagina, show suspected signs of underlying chlamydia infection.
Q3. How long does chlamydia last?
Chlamydia infection can last for years when neglected and left untreated. Being a bacterial infection, it will keep on worsening the afflicted area unless treated with antibiotic therapy.
Q4. Does chlamydia have a smell?/Do chlamydia symptoms have a characteristic smell?
The most characteristic chlamydia symptoms include smelly and sticky discharge from the urethra and vagina. Besides, patients experience pelvic inflammation (women) and intense pain in the testis (men).
Q5. Can chlamydia go away without treatment?/Can chlamydia go away naturally?
Chlamydia is a bacterial infection contracted sexually, meaning it’s unlikely to go away naturally unless reduced through a preventive lifestyle or cured through antibiotic therapy.