Filter :
हार्मोनल असंतुलन के कारण पुरुष में कई तरह की समस्याएं पैदा होती हैं। गाइनेकोमैस्टिया भी उन्हीं में से एक है। यह एक सामान्य बीमारी है जो पुरुषों को यौवन के दौरान और बुढ़ापें में प्रभावित करती है।
Table of Contents
गाइनेकोमैस्टिया को मैन बूब्स के नाम से भी जाना जाता है। यह पुरुषों में होने वाली एक आम समस्या है जिससे पीड़ित पुरुष के स्तनों का आकार सामान्य से अधिक बढ़ जाता है। स्तनों का आकार बढ़ने के कारण वे महिलाओं के स्तनों की तरह दिखाई पड़ते हैं।
गाइनेकोमैस्टिया बिलकुल महिलाओं के स्तनों की तरह नहीं होता है, लेकिन कुछ मामलों में उनसे मिलता-जुलता होता है। गाइनेकोमैस्टिया पुरुष के पर्सनल और प्रोफेशनल दोनों जीवन को बुरी तरह से प्रभावित करता है।
शोध के मुताबिक, इस समस्या से पीड़ित लड़के अक्सर अपने ग्रुप में मजाक का पात्र बन जाते हैं। गाइनेकोमैस्टिया के कारण एक लड़के का आत्मविश्वास बहुत कम हो सकता है। यह कोई जानलेवा समस्या नहीं है, लेकिन जीवन की गुणवत्ता को कई तरह से प्रभावित कर सकता है।
यही कारण है कि यह समस्या होने पर तुरंत डॉक्टर से परामर्श करना चाहिए। उचित जांच और इलाज की मदद से उसको आसानी से दूर किया जा सकता है।
ये भी पढ़े: हार्ट अटैक के स्टेज और उनका इलाज
गाइनेकोमैस्टिया कई कारणों से होता है जिसमें सबसे पहला हार्मोन में असंतुलन होना है। हार्मोन में असंतुलन होने पर एस्ट्रोजन की तुलना में टेस्टोस्टेरोन हार्मोन का स्तर काफी कम हो जाता है।
आमतौर पर पुरुष बहुत कम मात्रा में एस्ट्रोजन हार्मोन का उत्पादन करते हैं, लेकिन जब एस्ट्रोजन हार्मोन का स्तर बहुत अधिक होता है तो गाइनेकोमैस्टिया की समस्या पैदा हो सकती है।
गाइनेकोमैस्टिया के कारणों में यौवन यानी 15-18 की उम्र और बुढ़ापा यानी 50-80 की उम्र शामिल हैं। इसके अलावा, ऐसी बहुत सी दवाएं हैं जो गाइनेकोमैस्टिया का कारण बन सकती हैं। इसमें शामिल हैं:-
निम्नलिखित पदार्थों का सेवन गाइनेकोमैस्टिया का कारण बन सकता है:-
कुछ ऐसी भी स्वास्थ्य स्थितियां है जिनके कारण गाइनेकोमैस्टिया की शिकायत हो सकती है। इसमें निम्न शामिल हो सकते हैं:-
ये भी पढ़े: जानिए काला पीलिया क्यों होता है ? इसके कारण, लक्षण, उपचार
गाइनेकोमैस्टिया के लक्षणों में शामिल हैं:-
ये भी पढ़े: उच्च रक्तचाप का कारण, लक्षण और इलाज
गाइनेकोमैस्टिया का उपचार इसके ग्रेड पर निर्भर करता है। कुछ मामलों में उपचार की आवश्यकता नहीं पड़ती है। अगर गाइनेकोमैस्टिया अपनी शुरुआती स्टेज में है तो डॉक्टर मरीज को जीवनशैली और डाइट में कुछ सकारात्मक बदलाव लाने का सुझाव देते हैं।
इसमें समय पर नींद सोना और जागना, अपनी डाइट में हरी पत्तेदार सब्जियों और ताजे फलों को शामिल करना, रोजाना सुबह और शाम हल्का-फुल्का व्यायाम करना, शराब, सिगरेट या दूसरी नशीली चीजों के सेवन से बचना शामिल है।
इसके अलावा, डॉक्टर फास्ट फूड और कोल्ड ड्रिंक के अत्याधिक सेवन से बचने का भी सुझाव देते हैं। डाइट और लाइफस्टाइल में बदलाव लाने के बाद फायदा नहीं होने या गाइनेकोमैस्टिया का ग्रेड-3 होने पर डॉक्टर दवाएं और सर्जरी का उपयोग करते हैं।
गाइनेकोमैस्टिया की सर्जरी को दो तरह से किया जाता है जिसमें पहला लिपोसक्शन और दूसरा मेसाटेक्टोमी है। लिपोसक्शन के दौरान, सर्जन एक्स्ट्रा फैट को बाहर निकाल देते हैं। इस सर्जरी के दौरान स्तन की ग्रंथियों को नहीं हटाया जाता है।
हालांकि, मास्टेक्टोमी के दौरान स्तनों की ग्रंथियों को निकाल दिया जाता है। आमतौर पर इस सर्जरी को एंडोस्कोपी की मदद से किया जाता है।
निम्न बातों का पालन करके गायनेकोमैस्टिया को रोका जा सकते है:-
ये भी पढ़े: पुरुषो में किडनी स्टोन (गुर्दे की पथरी): लक्षण, कारण, और उपचार
प्रश्न 1. क्या गायनेकोमैस्टिया को ठीक किया जा सकता है?
हां, गायनेकोमैस्टिया को ठीक किया जा सकता है। इसके उपचार के अनेक तरीके मौजूद हैं जिसमें एक्सरसाइज, डाइट, दवाएं और सर्जरी शामिल हैं।
प्रश्न 2. क्या मैन बूब्स का कारण जेनेटिक हो सकता है?
हां, शोध के मुताबिक कुछ लोगों में जेनेटिक कारणों से गायनेकोमैस्टिया हो सकता है।
प्रश्न 3. गाइनेकोमैस्टिया सर्जरी कैसे होती है?
आमतौर पर गायनेकोमैस्टिया की सर्जरी को दो तरह से किया जाता है जिसमें पहला लिपोसक्शन और दूसरा मास्टेक्टोमी है। इस सर्जरी के दौरान , स्तन के आसपास एक छोटा सा चीरा लगाकर वहां मौजूद एक्स्ट्रा फैट को बाहर निकाल दिया जाता है।
Table of Contents
A seven-year-old boy visited the Department of GI, Minimal Access & Laparoscopic Surgery at the CK Birla Hospital, Delhi.

He had complaints of severe abdominal pain that had been affecting him for the last 3 years. The patient was also reported to be hospitalised several times for pain management.
Dr Amit Javed, a leading laparoscopic G.I.surgeon attended to the patient and evaluated his condition. Dr Amit suggested a few tests and screenings to precisely diagnose the condition.
The findings revealed that the patient had multiple strictures in the pancreatic duct along with the presence of multiple stones in the pancreas. He was also suffering from bile duct obstruction. After analysing the findings of the tests, Dr Amit went ahead with the laparoscopic surgery as this was the best treatment for the patient.
The patient had visited various other hospitals earlier seeking relief. However, he was denied surgical intervention due to his age and low weight (17 kgs). Moreover, Dr Amit decided to perform laparoscopic surgery to treat the patient.
The surgical team at the CK Birla Hospital, led by Dr Amit, successfully performed a complex laparoscopic surgery to treat the patient. Using the laparoscopic technique, the team of surgeons opened the entire pancreatic duct and removed the stones surgically. After that, the team created a new passage for the uninterrupted flow of pancreatic juice and bile juice.
After performing the surgery, Dr Amit stated “Only a handful of cases of laparoscopic surgery in small children have ever been reported and this is probably the first in India.” A minimally invasive surgical procedure such as laparoscopy is rarely used to treat chronic pancreatitis and associated bile duct stricture.
Dr Amit is an expert Gastrointestinal, Gastrointestinal Cancer, Laparoscopic & Bariatric/ Weight Loss Surgeon with over 20 years of experience. He is skilled in minimally invasive/laparoscopic surgeries and has been a mentor to many budding surgeons. He was also the first in India to perform Whipple’s Surgery to cure pancreatic cancer in a 6-month pregnant lady.
The surgical procedure was completed without any complications and the child recovered quickly. He was closely monitored by the surgical team and discharged from the hospital after 4 days of the surgery.
The patient greatly benefitted from laparoscopic surgery that offered him quick and long-term relief, allowing him to lead a normal, healthy and happy life.
Benefits of laparoscopic surgery include:-
Pancreatitis is the inflammation of the pancreas, which is a long, flat gland that sits tucked behind the stomach in the upper abdomen. The pancreas produces enzymes that help digestion and hormones, helping regulate the way the body processes sugar. Pancreatitis can occur as acute pancreatitis that appears suddenly and last for days.
However, some people may develop chronic pancreatitis that occurs for many years. Mild pancreatitis improves with treatment. However, severe cases can cause life-threatening complications. The most common symptoms of chronic pancreatitis may include:-
Chronic pancreatitis can impair the flow of pancreatic juice leading to severe abdominal pain. Bile duct stricture impairs the flow of bile leading to jaundice. Pancreatitis is a life-threatening condition if left untreated.
Recurrent pancreatitis may cause blood and fluid loss causing life-threatening conditions such as multi-organ failure. Therefore, timely medical intervention and proper treatment are needed.
At the Department of GI, Minimal Access & Bariatric Surgery, CK Birla Hospital, we offer a comprehensive range of surgical treatments including surgeries for cancer, general and gastrointestinal, and breast and obesity for both women and men.
Our doctors are trained in the latest minimally invasive laparoscopic procedures to treat a wide spectrum of conditions, ensuring that recovery time is considerably minimized. Precision in diagnosis and treatment is of paramount importance to us.
Our team of surgeons, anesthetists, intensivists and nurses use the latest equipment and innovative procedures to ensure accuracy, safety and the best clinical outcomes.
We offer:-
If you experience the symptoms of pancreatitis or suffering from any gastrointestinal diseases or disorders, and seeking the most effective and personalized treatment, you can book an appointment and consult our doctors now.
हाइड्रोसील (Hydrocele in Hindi) पुरुषों को प्रभावित करने वाली एक सामान्य समस्या है। इससे पीड़ित पुरुष के अंडकोषों में पानी भर जाता है, जिसके कारण अंडकोष में सूजन आ जाती है।
हाइड्रोसील किसी भी पुरुष को हो सकता है, लेकिन अधिकतर मामलों में यह 40 से अधिक उम्र के पुरुषों में देखा जाता है।
ये भी पढ़े: पेशाब में जलन क्या है – कारण, निदान और उपचार
Table of Contents
हाइड्रोसील पुरुष के अंडकोष में होने वाली एक आम समस्या है जिसमें अंडकोष में द्रव यानी पानी जमा हो जाता है। हाइड्रोसील के कारण अंडकोष का आकार बढ़ जाता है और उसमें दर्द भी हो सकता है।
डॉक्टर के मुताबिक, छोटे बच्चों को हाइड्रोसील हो सकता है, लेकिन यह कुछ समय के अंदर अपने आप ठीक हो जाता है। हालांकि, वयस्कों में उपचार की आवश्यकता होती है। हाइड्रोसील का उपचार करने के लिए अंडकोष में जमा पानी को बाहर निकाला जाता है।
हाइड्रोसील अंडकोष में चोट लगने, नसों में सूजन आने या स्वास्थ्य से संबंधित किसी प्रकार की समस्या, ज्यादा शारीरिक संबंध बनाने, हेवी एक्सरसाइज करने, भारी वजन उठाने या दूसरे अन्य कारणों से हो सकता है।
ये भी पढ़े:
हाइड्रोसील दो प्रकार के होते हैं जिसमें पहला कम्युनिकेटिंग हाइड्रोसील और दूसरा नॉन कम्युनिकेटिंग हाइड्रोसील है।
इस तरह का हाइड्रोसील होने पर अंडकोष की थैली पूर्ण रूप से बंद नहीं होती है और इसमें सूजन एवं दर्द होता है। हर्निया से पीड़ित मरीज में कम्युनिकेटिंग हाइड्रोसील का खतरा अधिक होता है।
इस स्थिति में अंडकोष की थैली बंद होती है और बचा हुआ द्रव शरीर में जमा हो जाता है। इस प्रकार का हाइड्रोसील नवजात शिशुओं में अधिक देखने को मिलता है और कुछ समय के अंदर यह अपने आप ही ठीक हो जाता है।
हाइड्रोसील कई कारणों से होता है। हम आपको नीचे हाइड्रोसील के कुछ मुख्य कारणों के बारे में बता रहे हैं।
अधिकतर बच्चों में हाइड्रोसील की समस्या जन्म के समय से होती है। समय से पहले जन्मे बच्चों में इसका खतरा अधिक होता है। इसके अलावा, हाइड्रोसील के अन्य कारणों में निम्न शामिल हो सकते हैं:-
हाइड्रोसील के अनेक लक्षण (Hydrocele Symptoms) होते हैं जिनकी मदद से आप या आपके डॉक्टर इस बात की पुष्टि कर सकते हैं कि आपको हाइड्रोसील है। हाइड्रोसील के निम्न लक्षण हो सकते हैं:-
अगर आप ऊपर दिए गए लक्षणों को खुद में अनुभव करते हैं या हाइड्रोसील से पीड़ित हैं तो आपको डॉक्टर से परामर्श करना चाहिए।
हाइड्रोसील का निदान करने के लिए डॉक्टर मरीज का शारीरिक परीक्षण करते हैं और साथ ही कुछ जांच करने का सुझाव देते हैं।
शारीरिक परीक्षण में निम्न शामिल हैं:-
हाइड्रोसील की जांच करने के लिए डॉक्टर खून और मूत्र परीक्षण एवं अल्ट्रासाउंड करने का सुझाव देते हैं।
इन जांचों की मदद से डॉक्टर यह निर्धारित करते हैं कि मरीज को एपिडिडीमाइटिस जैसा संक्रमण तो नहीं है।
अंडकोष में ट्यूमर और सूजन एवं हर्निया का पता लगाने के लिए डॉक्टर अल्ट्रासाउंड करने का सुझाव देते हैं।
हाइड्रोसील का इलाज (Hydrocele Ka Ilaj) कई तरह से किया जाता है। इसमें मुख्य रूप से एस्पिरेशन और सर्जरी शामिल हैं। हाइड्रोसील की सर्जरी को हाइड्रोसिलोक्टोमी के नाम से भी जाना जाता है।
एस्पिरेशन के दौरान, डॉक्टर इंजेक्शन की मदद से अंडकोष में जमे द्रव को बाहर निकाल देते हैं। यह प्रक्रिया खत्म होने के बाद, डॉक्टर छेद को बंद करने के लिए स्क्लिरोजिंग नामक दवा को इंजेक्ट करते हैं।
ऐसा करने से दोबारा हाइड्रोसील होने का खतरा कम हो जाता है। हाइड्रोसील की सर्जरी के दौरान, डॉक्टर स्क्रोटम में छोटा सा कट लगाकर अंदर जमा हुए द्रव को बाहर निकाल देते हैं।
हाइड्रोसील की सर्जरी को पूरा होने में लगभर 20-30 मिनट का समय लगता है। सर्जरी ख़त्म होने के कुछ ही घंटों के बाद मरीज को हॉस्पिटल से डिस्चार्ज कर दिया जाता है।
हाइड्रोसील की सर्जरी के बाद मरीज को पूर्ण रूप से ठीक होने में लगभग 3-6 दिनों का समय लगता है।
अधिकतर मामलों में हाइड्रोसील को रोका नहीं जा सकता है। लेकिन कुछ बातें हैं जिन पर ध्यान देकर इसके खतरे को कम किया जा सकते हैं, जैसे कि क्रिकेट या दूसरे खेल के दौरान सुरक्षात्मक गियर पहनना ताकि अंडकोष पर चोट न लगे।
Since 2019, when the pandemic hit our lives, there hasn’t been one day when we did not hear about some of the other variants being released into our environment as if the Coronavirus wasn’t enough. One such injection called the Black Fungus, has not just spread like an infection but there have been so many assumptions that have spread regarding what exactly are the black fungus symptoms and how can one diagnose or get themselves treated for black fungus (also called Mucormycosis).
In this article, with the help of expert insights from Dr. Ravindra Gupta, a leading internal medicine specialist at The CK Birla Hospital, we will understand what is a black fungus, its symptoms and why COVID patients are being affected by it.
Table of Contents
Black fungus is a non-contagious yet serious and rare fungal infection that if not treated can be fatal. It is mostly found and detected in people who have earlier been infected with coronavirus, viral infectious diseases, immunodeficiency diseases, cancer and other medical conditions. Mucormycosis, or black fungus, is caused by fungi called mucormycetes, which are found in the environment, especially in soil and in conjunction with decaying organic substrates, compost piles, animal faeces, rotting wood, and plant material. This can be seen on rotting fruits and aged bread as a black-coloured growth.
Researchers believe that this type of fungus could have a significant impact on the immune system, it affects the body’s immune system so much that the body becomes more susceptible to fungal infections. This infection, mucormycosis is considered an effect of covid-19, meaning it affects people who have recovered from coronavirus. In recent times, the number of cases of black fungus and the deaths associated with it has increased. Therefore, it is absolutely essential for recovered patients of coronavirus and other immunodeficiency disease patients to learn and understand more about black fungal infection so that they are able to recognise its signs and symptoms.
There are several types of black fungus that can affect parts of the body and lead to black fungal infection. Mucormycosis of the skin (Cutaneous), gastrointestinal mucormycosis, pulmonary (lung) mucormycosis, and rhino cerebral (brain and sinus) mucormycosis are all examples of Black Fungus. As a result, Mucormycosis symptoms vary depending on where the fungus is germinating in your body.
(Infographics to be made for each mucormycosis symptom)
Mucormycosis is a rare yet fatal fungal infection which attacks the blood vessels and damages the body leading to severe complications like causing tissue necrosis and even death. As per research, it has been found that this fungus starts emerging in the body after the usage of steroids given to coronavirus patients. The drugs given for treating coronavirus patients contain elements which trigger the onset of this fungus. There is no doubt that these medications help relieve the inflammation and manage the effect of covid-19 infection but it comes with severe repercussions, like affecting the body’s ability to fight other infections like mucormycosis.
There are several types of fungi that can cause mucormycosis. The most common types that cause mucormycosis are Rhizopus species and Mucor species. Other examples include Rhizomucor species, Syncephalastrum species, Cunninghamella bertholletiae, Apophysomyces, Lichtheimia (formerly Absidia), Saksenaea, and Rhizomucor.
To diagnose and test if the patient is infected with black fungus below are some vital steps that should be abided by the patient and the doctor.
After diagnosis, the black fungus needs to be treated with prescribed antifungal medicines. The doctors with the right medication can help stop the growth of the fungus and control the infection until it is completely destroyed. In severe cases, surgery might be recommended as it can help remove dead and infected tissues. Before moving ahead with surgery, the patient needs to be strong mentally and physically as the surgery involves removing parts of the body that are infected.
Mucormycosis infection occurs in people who have already been infected with some or the immunodeficiency diseases. Patients who take medicines that have potential to lower the ability of the immune system making it difficult to fight infection back with the fungus. When infected with COVID-19 the body becomes weak and more vulnerable to infection thereby leaving the immune system at risk. So, people recovering from Covid-19 are at a higher risk due to a weak immune system.
Ques 1. How black fungus spread?
It does not spread from person to person, even though it is a rare infection but a dangerous fungal infection.
Ques 2. How black fungus is caused for COVID patients?
COVID patients become more prone to infection because their immune system becomes weak and also there are times when the medicines given to the patients cause side effects. Therefore, there are chances of black fungus infecting patients recovered from COVID.
Ques 3. Is black fungus contagious?
No, black fungus is not contagious but is a dangerous infection which may even cause death or permanent damage to the body.
A health emergency never knocks on the door. A medical trauma or critical situation may present in the most unexpected way. During that time, experienced clinical intervention can be inaccessible for the time being. It is, thus, important for ordinary citizens to learn how to manage emergency situations, for instance, heart attacks. Knowing first aid in a heart attack can be a life-saving measure.
This article, written with insights from Dr. Rashi Khare, leading critical care specialist at the CK Birla Hospital, offers key information about first aid in heart attack.
Table of Contents
Heart attack, also known as myocardial infarction, is a condition that occurs when blood flow to the heart gets blocked. This blockage can be a result of long-term or gradual damage to the organ. Primarily, the accumulation of fat and cholesterol along with other substances may lead to the formation of plague in the arteries of the heart. The formation of a plague can rupture an artery and lead to the development of a blood clot. Furthermore, blood clotting and blockage can damage or destroy the heart muscles.
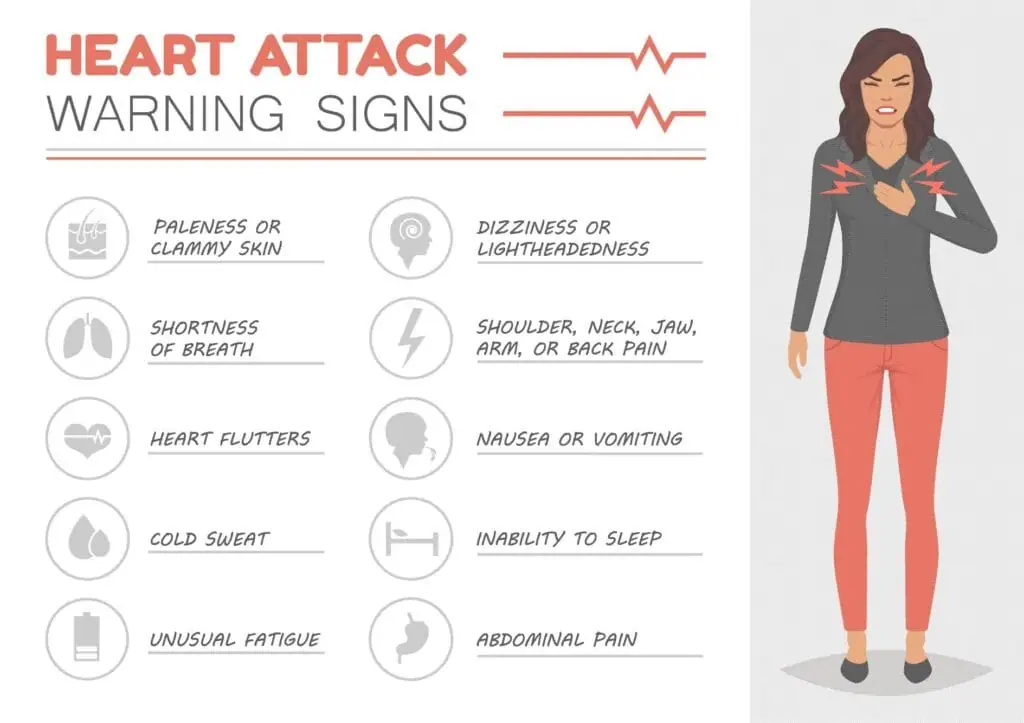
A medical emergency can look like and create a lot of panic. Before you deliver first aid in heart attack, you should at least know that the emergency situation is most likely the said disease. Therefore, it is important to learn about the common signs and symptoms of heart attack, which include:
It is to be noted that not everybody have similar symptoms of heart attack. Additionally, the intensity of the above-given symptoms also vary. It is also possible that some one may have only one symptom.
First aid for heart attack includes several precautionary steps. The following guide will help you cope with a stressful situation like this.

Step 1 – The first step you need to take when you suspect that somebody is having a heart attack is to call for help. You should instantly dial 112 and ask for an ambulance or connect with nearby healthcare institutions.
Step 2 – Analyze the affected person’s health condition and check if he/she is breathing. Additionally, check if the person has a pulse by examining the same on their wrist.
Step 3 (a) – In case the person is not breathing, you should immediately start CPR.
About CPR
CPR stands for Cardiopulmonary resuscitation. It is a life-saving measure that is provided to someone who is possibly having a heart attack or drowning.
CPR for heart attack can be performed by anyone – bystanders or first responders. Hands-only CPR includes giving repeated and rapid chest compressions in a rhythm of about 100-120 per minute until medical helpers arrive.
Step 3 (b) – If the person is not experiencing unconsciousness but has other obvious signs of heart attack, you should do the following:
If you are not a healthcare provider, the care and support you offer during the heart attack will be limited. While it is important to know which steps to take, it is essentially significant to know what not to do.
The following list provides an insight on what should be avoided while providing first aid in heart attack:
While in some people, heart attacks can occur suddenly, others may begin to notice their symptoms at least 2-3 days in advance.
Heart attack is a fatal condition, however, it can be effectively prevented with certain lifestyle recommendations and measures.
Here’s what you should do to reduce your chances of having a heart attack:
Timing is the key while providing first aid in a heart attack. You should act wisely and rapidly to help manage the person’s symptoms while professional medical health arrives.
The next steps for heart attack first aid are:
For more information and personalised guidance on first aid and critical care, visit the CK Birla Hospital.
Heart attack is one of the most known, common and fatal health concerns. Presently, it affects millions of people all over the world. This ailment also has a great mortality rate. Despite its high incidence, awareness and information about the fundamentals of this disease are lagging. In order to seek timely treatment and management, it is important to know about the symptoms and causes of heart attack.
In this article, with insights from our cardiologists, we will explore the most common reasons for heart attack. But before we dwell on the reasons, let us first study what this condition is all about?
Table of Contents
Heart attack is also known as myocardial infarction. It is a serious medical emergency that occurs when the blood flow to the heart gets blocked.
There is usually a formation of blood clots due to this blockage leading to complete disruption of blood supply. The blockage can not only disrupt the blood flow but also damage or destroy the organ due to an inadequate supply of oxygen.
A heart attack is characterised by a pressure, tightness, squeezing sensation or pain in the chest or arms, pain that radiates to the neck, jaw or back, nausea, indigestion, heartburn, abdominal pain, shortness of breath, cold sweating, fatigue, and sudden dizziness.
Cardiovascular diseases are highly common all across the globe. It is responsible for the deatlh of close to 17.9 million people worldwide. Out of these stark figures, 85% of the deaths are attributed to heart attack.
Also Read: Heart Valve Disease: Causes, Symptoms, and Treatment
Primarily, the reason for heart attack is the formation of plague caused by a build-up of fat, cholesterol and various other substances. The said plague forms in the arteries of the heart which is responsible for supplying oxygen-rich blood to the heart and causes the arteries to narrow.
Heart attack usually occurs as an effect of overtime damage to the organ. Overtime, due to sedentary lifestyle and other factors, one or more of the coronary arteries of the heart can get blocked due to the accumulation of fatty deposits (including cholesterol). This build-up leads to the development of a condition known as coronary artery disease which causes heart attack.
Heart attack is one such medically critical situation that can occur in anyone irrespective of their age or gender. However, some individuals or groups are at a greater risk of developing a complete or partial heart attack.
A range of factors – biological, lifestyle and others – can increase your chances of getting a heart attack some time. Common risk factors of heart attack are:
Also Read: Healthy Diet Chart for High Blood Pressure Patients
Heart attack, whether complete or partial, is a serious medical emergency. An episode of heart attack requires urgent and immediate critical care intervention. If not heeded timely, heart attack can lead to the following complications:
Points to note:
For more information on intensive care for heart attacks, you can speak to our healthcare providers. Book an appointment today.
Kidney stones are like tiny stones in the kidney which may seem tiny in size but the pain it causes is surely not tiny. Kidney stones leave excruciating pain in the side and back, below the ribs. It causes discomfort in the lower abdomen and groin. Pain from kidney stones comes in waves but varies in frequency. In people with kidney stones, the lower abdomen hurts like when a pregnant lady is having contractions and is being asked by the doctor to breathe.. stay calm.. you can do this.
Dr. Shalabh Agrawals, shares his views on how to dissolve kidney stones and what remedies can be followed to treat and prevent kidney stones.
Table of Contents
Before understanding how these kidney stones are formed it is important to know what kidney stones are. Kidney stones are hard deposits that form in the kidney and are often painful when passed through the ureters. They may be painful but they usually do not leave any permanent damage to the abdomen or the kidneys.
Once the kidney stones are formed, they result in severe pain in the abdomen, it may also affect the flow of urine with blood in urine, feeling nauseated, and vomiting. The stones pass down the urethra and may result in frequent urination, constant pain, and pressure in the bladder.
People who have kidney stones feel unbearable pain and all they want is to find an easy yet permanent solution for the kidney stones. Below are some of the things that can help relieve the pain caused due to kidney stones.
Increase your fluids intake as it can aid you in a variety of ways. It detoxifies the body and helps in the passage of stones through the urethra. Many times, even doctors will advise that the best way to treat kidney stones is to drink enough water throughout the day. Increased liquid intake can help shift the stone and remove the grit from the kidney stone. Drink as much water as you can because water is usually considered the best cure for many ailments. Water in itself can do wonders to the body. Other beneficial liquids are lemon water, being citric it can help break stones into small pieces and thereby speeding up the passage process of stones. Apple cider vinegar, again being citric in nature, can surely act as a game-changer for many, it helps to relieve pain and can add to other benefits as well. It boosts the process of flushing the stones out of the system.
Cut down on the intake of sodium and protein as it may boost uric acid in the body and further increase the chances of formation of kidney stones. Diet high in sodium can increase the risk of calcium in your urine, which can induce kidney stones. For those who are prone to stone formation, a low-sodium diet is recommended.
Signs are symptoms of kidney stones should be well observed and not ignored or else it can lead to severe unbearable pain in the abdomen. Kidney stones are like they can be in your kidney for years and still not cause any discomfort but when it starts to move or enlarge you may develop symptoms.
If your healthcare provider suspects that the pain around your abdomen or near ribs is due to kidney stones he/she will suggest a list of tests and procedures. Before proceeding with the tests the doctor will require your medical history in order to prescribe the tests
Basil being high in acetic acid and rich in nutrients helps to break down the kidney stones and relieve the pain. Basil is known to help relieve the discomfort caused due to digestive and inflammatory disorders. Basil is filled with antioxidants and anti-inflammatory substances which can help maintain kidney health.
As mentioned above, water is a savior and is truly the world’s first and foremost medicine. Water is both a driving force of nature and our body. Barley water helps to lower cholesterol, is good for kidneys and helps to flush out toxins from the body.
Pomegranate is known for being rich in antioxidants and has been used for years to improve the overall health of the kidney. Taking care of the kidney may eventually prevent the formation of stones in the kidney. It helps to flush out all the toxins from the system. Kidney stones are crystals made of calcium and uric acid, pomegranate juice helps to lower uric acid levels and thereby reducing the risk of further deterioration of stones.
Kidney bean soup has been known to improve kidney health. It aids to dissolve and flush out any toxins of the stones.
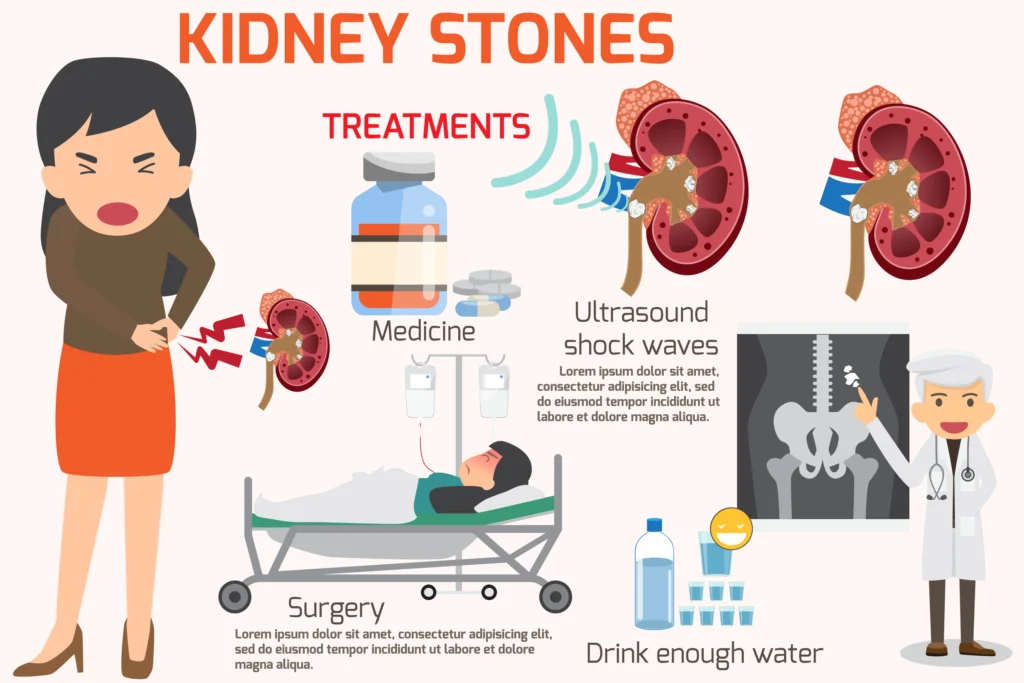
The kidney stones that are small in size can be taken care of with home remedies or as per doctors’ suggestion. But the other stones, that are large in size and are in a difficult position may be taken out through surgical methods.
Ques 1. How do you dissolve hard kidney stones?
The doctor may give shock therapy to break hard stones into small pieces so that they can easily be flushed out of the system
Ques 2. How can I force a kidney stone to pass at home?
Drinking loads of fluids, like water or drinks rich in citric acid like orange, apple cider vinegar may help to encourage the stones to pass at home.
Ques 3. How much apple cider vinegar should I drink to dissolve kidney stones?
Add 1-2 tablespoons of apple cider to water and drink. Being citric in nature can help dissolve kidney stones.
Ques 4. How do I know if my kidney stone is moving?
If your stones are moving towards your groin, you might start feeling a slight urgency to urinate.
Ques 5. How do you sleep with a kidney stone?
The right posture to sleep if you have a kidney stone is on the side where the stone is as this may help move the stone. Also, if the pain becomes unbearable, seek immediate medical help.
Kidneys are vital organs in your body. The bean-shaped organs are responsible for filtering waste and extra fluids from your body as well as maintaining a healthy balance of salts, minerals and water. Having kidney disease can affect your general health.
It is, thus, important to take extra care of your body if you are experiencing kidney disease. The top factor in maintaining your overall health is your dietary intake. A diet chart for kidney patients is an important tool that provides key details about what to eat and what to avoid.
In this article, with insights from Dr. Mohit Khirbat, a leading nephrologist at the CK Birla Hospital, we will explore the chronic kidney disease diet food list. But first, let’s begin by understanding what kidney disease is?
Table of Contents
Your kidneys are responsible for removing excess fluids and waste from your blood. This wastage is then converted into urine which is drained from the body.
Kidney disease is a condition that leads to the loss of kidney function and restricts your body to lose extra waste as it should. It can be an acute or chronic condition. Kidney disease is characterised by a range of varying symptoms. Common signs and symptoms of chronic kidney disease include:
Chronic kidney disease (CKD) is a highly prevalent condition. It is estimated that about 697.5 million individuals were recorded to have chronic kidney disease in 2017 alone, making up for a 9.1% global incidence.
If you are suffering from chronic kidney disease, your body’s ability to filter waste is compromised. It means that your kidneys are unable to perform their function properly. Hence, you should ensure to eat included in the Indian diet chart for kidney patients so that your kidneys are able to function healthily despite kidney disease.
Modifying your kidney diet chart can help you avoid complications of kidney disease and improve your quality of life.
In addition, a proper diet chart for high creatinine patient provides:
Also Read: Healthy Diet Chart for High Blood Pressure Patients
Before we jump into understanding food for dialysis patients, we should learn what dialysis is all about.
Since kidneys are unable to filter any waste while experiencing kidney disease, a novel treatment for kidney patients. Dialysis is a procedure in which a machine is used to filter and remove waste products. A dialysis machine also regulates minerals and salts in your blood and controls blood pressure.
There are two types of dialysis:
Dialysis does not cure kidney disease but only offers temporary relief and allows your body to get rid of waste and extra fluids.
Also Read: Kidney Dialysis: Types, Risks & Outlook
A personalised dialysis patient diet chart can help someone with kidney disease relieve their symptoms and live a better quality of life. An ideal renal diet should be low in sodium, protein and phosphorus. In some patients, an additional restriction on the intake of calcium and potassium is also there.
Maintaining the balance of these nutrients is important in order to eat a healthy diet as well as keep the kidney disease from progressing further.
Listed below are the top components you should include in the diet chart for kidney patients:
Sodium is a mineral found in salt and is used as a common seasoning. A kidney patient should avoid consuming higher levels of sodium. Intaking higher levels of salt can increase your thirst, blood pressure levels, and further cause swelling in the legs, hands and face. Low levels of salt, on the other hand, can help regulate blood pressure levels, nerve function and muscle contraction.
How to monitor sodium intake: Read food labels, choose fresh fruits and vegetables, and avoid consumption of packaged meats.
Potassium is a mineral that occurs naturally in the body. It is also found in several food items. Potassium is important for muscle function and regulating heartbeat. It, additionally, improves fluid and electrolyte balance in the blood.
It is important for kidney patients to balance their potassium intake as high levels of this mineral in your blood can lead to muscle weakness, irregular heartbeat and slow pulse.
How to monitor potassium intake: Limit the consumption of foods high in potassium, choose fresh fruits and vegetables, and avoid salt substitutes.
Phosphorus is important for bone development and strength. It also helps in maintaining muscle function and the development of connective tissue. If you are a kidney patient, your ability to filter phosphorus decreases. When your kidneys are not functioning at their full potential and you consume high levels of phosphorus, your body can pull out extra calcium from your bones and cause calcium deposits in the blood vessels and various organs.
How to monitor phosphorus intake: Choose foods that are low in phosphorus, avoid packaged foods, and eat smaller portions of food high in protein.
Damaged kidneys are unable to filter protein from food, which in turn, gets collected in the blood. Protein, however, plays a significant role in tissue maintenance. Therefore, it is important to balance your protein intake.
How to monitor protein intake: Check labels, avoid consumption of processed foods and maintain a food journal.
Fluids are essential for your body’s hydration. However, if you are suffering from kidney disease, you are required to balance your fluid intake so that the dialysis can fully filter the waste from your body. High fluid intake can increase the pressure on your heart and lungs.
It is important to maintain your fluid intake based on your urine output as well as your dialysis setting.
How to monitor fluid intake: Avoid drinking additional fluids and be aware of the amount of water you keep while cooking.
| Foods good for kidneys | Foods bad for kidneys |
| Fruits (peaches, grapes, pears, apples, berries, pineapple, plums, tangerines, and watermelon) | Oranges and orange juice, nectarines, kiwis, raisins or other dried fruit, bananas, cantaloupe, honeydew, and prunes |
| Grains, Dalia, & oatmeal | Nuts |
| Olive oil, canola oil and safflower oil | Chocolate |
| Fish, poultry and eggs | Dark-coloured soda, processed food, pickles, tomatoes, and ready-to-eat meals |
| Milk, yoghurt and cheese | High-fat dairy products |
| Vegetables (broccoli, cabbage, carrots, cauliflower, celery, red pepper, cucumber, eggplant, green and wax beans, lettuce, onion, peppers, watercress, zucchini, and yellow squash) | Asparagus, avocado, potatoes, tomatoes or tomato sauce, winter squash, pumpkin, and cooked spinach |
Diet chart for kidney patients is a significant and handy tool that can help kidney patients lead a life of good quality.
For more information or personalised guidance on kidney disease, you can book an appointment with Dr. Mohit Khirbat, a leading nephrologist at the CK Birla Hospital, Gurgaon.
Also Read: Renal Failure (Kidney Failure): Causes, Symptoms, Diagnosis, and Treatment
Ques 1. What are the 10 best foods for kidney disease?
The 10 best foods for kidney disease are broccoli, cabbage, carrots, cauliflower, celery, red pepper, cucumber, eggplant, green and lettuce.
Ques 2. Which food reduces creatinine level?
To reduce creatinine levels, reduce your consumption of red meat and fish.
Ques 3. What fruit is good for the kidneys?
Peaches, grapes, pears, apples, berries, pineapple, plums, tangerines, and watermelon are good fruits for kidneys.
मिनिस्कस टियर (Meniscus Tear in Hindi) एक गंभीर समस्या है जिसके कारण आपको तेज दर्द और अनेक परेशानियों का सामना करना पड़ सकता है।
घुटना शरीर के अहम् जोड़ों में से एक है जो दैनिक जीवन के उन सभी कामों को आसानी से पूरा करने में मदद करता है जिसमें घुटने की भूमिका शामिल है। चलते, दौड़ते, ऊंचाई से कूदते या दैनिक जीवन की दूसरी गतिविधियों को करते समय घुटने में चोट आ जाती है, मिनिस्कस टियर भी उन्हीं में से एक है।
मिनिस्कस टियर को मेनिस्कस टियर के नाम से भी जाना जाता है। आइए इस ब्लॉग में मेनिस्कस टियर के कारण, लक्षण और इलाज के बारे में विस्तार से जानने की कोशिश करते हैं।
Table of Contents
घुटने की नरम उपास्थि यानी कार्टिलेज में लगी चोट को मेडिकल भाषा में मिनिस्कस टियर कहते हैं। मिनिस्कस घुटने की कार्टिलेज का एक हिस्सा है जो घुटने की जोड़ को स्थिर रखता है। यह हड्डियों को घिसने से बचाने का भी काम करता है।
वैसे तो मिनिस्कस टियर किसी को भी हो सकता है, लेकिन अधिकतर मामलों में यह खिलाड़ियों में देखने को मिलता है। क्रिकेट, फुटबॉल, हॉकी, वॉलीबॉल या दूसरे खेल के दौरान अक्सर चोट लगने पर मिनिस्कस टूट या फट जाता है।
कई बार चलते या दौड़ते समय अचानक से अपनी दिशा बदलने के कारण भी मिनिस्कस टियर हो सकता है। इतना ही है, उम्र बढ़ने पर घुटने का कार्टिलेज कमजोर हो जाता है जिसके कारण मिनिस्कस टियर का खतरा बढ़ जाता है।
मिनिस्कस का जांच करके इसकी चोट की गंभीरता की जांच की जाती है। जांच के बाद, डॉक्टर मिनिस्कस टियर के कारण और गंभीरता के आधार पर उपचार का चयन करते हैं। मिनिस्कस टियर का इलाज कई तरह से किया जा सकता है।
मिनिस्कस आमतौर पर अचानक मूवमेंट के कारण होता है। जब घुटने को उसकी क्षमता से अधिक अचानक से मोड़ दिया जाता है तो मिनिस्कट टूट जाता है।
साथ ही, लंबे समय तक घुटने पर भार देने या खेलकूद के दौरान अचानक से घुटने में चोट लगने के कारण भी मिनिस्कस टियर की समस्या हो सकती है।
उम्र बढ़ने पर उत्तक कमजोर हो जाता है जिसके कारण मिनिस्कस टियर हो सकता है। उम्र बढ़ने पर कार्टिलेज कमजोर हो जाती है जिसकी वजह से एक साधारण मूवमेंट भी मिनिस्कस टियर का कारण बन सकता है।
मिनिस्कस में चोट लगने या उसके फटने पर कुछ लोगों को घुटने में चटक की आवाज आ सकती है। साथ ही, कुछ लक्षण भी दिखाई दे सकते हैं जैसे कि:-
इन सबके अलावा, सीढ़ी चढ़ने-उतरने, घुटने को मोड़ने या दैनिक जीवन के दूसरे उन सभी कामों को पूरा करने में परेशानी होना जिसमें घुटने का इस्तेमाल शामिल है।
अगर आप ऊपर दिए गर लक्षणों को खुद में अनुभव करते हैं तो जल्द से जल्द एक हड्डी रोग विशेषज्ञ से परामर्श करना चाहिए।
मिनिस्कस टियर का निदान आवश्यक है, क्योंकि इसी से डॉक्टर मिनिस्कस टियर के कारण और गंभीरता एवं जटिलताओं की पुष्टि करते हैं।
मिनिस्कस टियर का निदान करने के लिए डॉक्टर अनेक जांच का सुझाव दे सकते हैं। सबसे पहले डॉक्टर मरीज का शारीरिक परीक्षण करते हैं। शारीरिक परीक्षण के दौरान डॉक्टर घुटने की गतिशीलता की जांच करते हैं। शारीरिक परीक्षण करने और लक्षणों से संबंधित कुछ प्रश्न पूछने के बाद डॉक्टर कुछ जांच करने के सुझाव दे सकते हैं जिसमें निम्न शामिल हैं:-
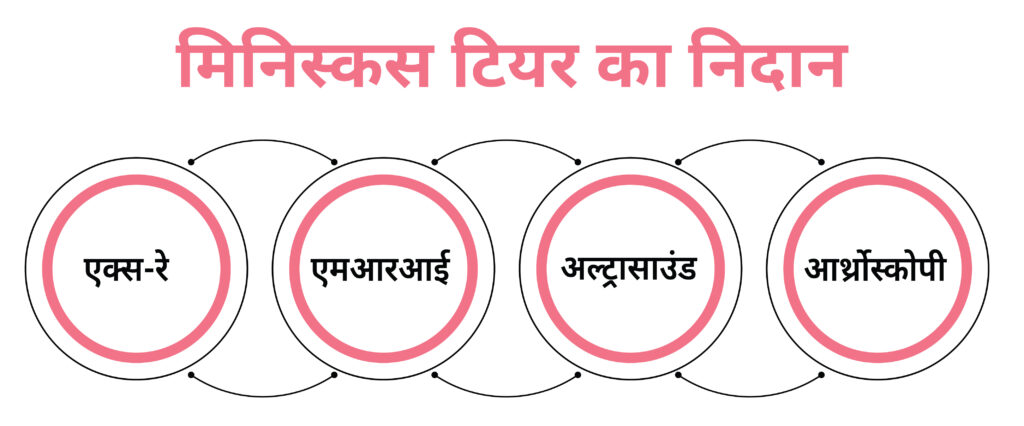
एक्स-रे की मदद से डॉक्टर मिनिस्कस टियर की पुष्टि कर सकते हैं। एक्स-रे से डॉक्टर इस बात का पता भी लगाते हैं कि घुटने में दर्द का कारण ऑस्टियोअर्थराइटिस तो नहीं है।
एमआरआई के दौरान डॉक्टर कार्टिलेज और लिगामेंट की तस्वीर लेकर इस बात की पुष्टि करते हैं कि मिनिस्कस में टियर है या नहीं।
अल्ट्रासाउंड के दौरान डॉक्टर इस बात का पता लगाते हैं कि घुटने की कार्टिलेज में ढीलेपन तो नहीं है।
अगर एक्स-रे, एमआरआई या अल्ट्रासाउंड के बाद भी घुटने के दर्द के कारण की पुष्टि नहीं होती है तो डॉक्टर आर्थ्रोस्कोपी का उपयोग करते हैं।
इन सभी जांच के परिणाम आने के बाद, डॉक्टर मिनिस्कस टियर के कारण और गंभीरता एवं मरीज की उम्र तथा समग्र स्वास्थ्य को ध्यान में रखते हुए उपचार के माध्यम का चयन कर इलाज शुरू करते हैं।
मिनिस्कस टियर का इलाज कई तरह से किया जाता है। इसके उपचार के माध्यमों में निम्न शामिल हो सकते हैं:-
मिनिस्कस में चोट लगने पर डॉक्टर सबसे पहले मरीज को आराम करने का सुझाव देते हैं। साथ ही, पैर का इस्तेमाल कम से कम या न के बराबर करने को कहते हैं।

मेनिस्कस टियर के कारण उत्पन्न दर्द और सूजन को कम करने के लिए डॉक्टर बर्फ से घुटने की सिकाई करने का सुझाव दे सकते हैं।
घुटने के दर्द और सूजन को करने के लिए डॉक्टर कुछ खास दर्द निवारक दवाएं भी निर्धारित कर सकते हैं।
मिनिस्कस टियर के लक्षण को दूर और घुटने के आसपास की मांसपेशियों को मजबूत करने के लिए डॉक्टर शारीरिक चिकित्सा का भी सुझाव दे सकते हैं।
शारीरिक चिकित्सा घुटने के दर्द को कम करने के साथ-साथ घुटने की गतिशीलता एवं स्थिरता को बढ़ाने में मदद भी करता है।
घुटने के दर्द को दूर करने के लिए डॉक्टर घुटने की मालिश करने का भी सुझाव दे सकते हैं।
जब ऊपर बताए गए उपायों से कोई फायदा नहीं होता है या मिनिस्कस बुरी तरह से चोट आता है तो डॉक्टर सर्जरी का उपयोग करते हैं।
मिनिस्कस टियर का उपचार करने के लिए जिस सर्जरी का उपयोग किया जाता है उसे आर्थ्रोस्कॉपी सर्जरी कहते हैं।