Filter :
Osteomalacia, often referred to as “soft bones,” is a metabolic bone disorder characterised by a deficiency in vitamin D, calcium, or phosphate, leading to weakened and softened bones. This condition primarily affects adults and can result in bone pain, fractures, and muscle weakness.
Understanding its causes, symptoms, diagnosis, and treatment options is crucial for effectively managing and preventing its debilitating effects on skeletal health.
Table of Contents
Osteomalacia, which translates to “soft bones,” is a condition characterised by weakened bones that are more susceptible to fractures. This disorder arises from decreased mineralization, leading to a breakdown of bone structure at a faster rate than it can regenerate.
Osteomalacia primarily affects adults, whereas insufficient vitamin D levels in children can lead to a similar condition known as rickets. This ailment differs from osteoporosis. Osteoporosis entails the deterioration of existing living bone undergoing remodelling.
Osteomalacia manifests through various symptoms:
These symptoms collectively signify the presence of osteomalacia, warranting medical attention and intervention.
You Can Also Read: Chondromalacia Patella: Causes, Symptoms and Treatment
Osteomalacia, primarily caused by a lack of vitamin D, is a condition where bones become soft and weak. Key points include:
Factors contributing to vitamin D deficiency:
Conditions affecting vitamin D absorption:
Other contributing factors:
Your healthcare provider diagnoses osteomalacia through blood tests, X-rays, and possibly a bone biopsy:
Overall, blood tests and X-rays usually suffice for diagnosis, with biopsies reserved for confirmation when needed. This all-inclusive method guarantees a precise diagnosis and suitable therapy.
You Can Also Read: High Tibial Osteotomy
Treatment for osteomalacia involves addressing underlying causes and supplementing with vitamin D and calcium:
Untreated or severe osteomalacia presents several complications:
Timely diagnosis and treatment are crucial to mitigate these complications.
You Can Also Read: Osteochondritis Dissecans (OCD)
Preventing osteomalacia involves a combination of lifestyle measures and dietary choices:
Maintaining a healthy weight, limiting alcohol and caffeine, quitting smoking, and regular medical monitoring are essential. Consult healthcare providers for personalised advice and bone density
Osteomalacia is a condition marked by softening of the bones, often due to vitamin D deficiency. Early diagnosis and proper treatment are crucial for managing symptoms and preventing complications. It is always advisable to seek medical help from an experienced orthopaedist. Timely care and help can ensure an appropriate diagnosis and treatment of your condition.
At the CK Birla Hospital, we ensure patients get holistic medical support which includes treatment in a compassionate environment. This patient-centric approach not only helps patients heal better but also ensures they are aware of the preventive measures as well. In case you need to consult an orthopaedist, reach out to us, or book a direct appointment at the CK Birla Hospital.
Yes, osteomalacia can occur in children. It’s a condition characterised by softening of bones due to vitamin D deficiency or other factors affecting bone mineralization during growth.
Risk factors for osteomalacia include inadequate sunlight exposure, insufficient dietary intake of vitamin D, malabsorption disorders, renal diseases, certain medications, and conditions affecting the metabolism of vitamin D or calcium.
Yes, prolonged untreated osteomalacia can lead to osteoporosis. Both conditions involve decreased bone density, but osteomalacia specifically results from a lack of mineralization due to vitamin D deficiency.
Yes, certain medications such as anticonvulsants, glucocorticoids, proton pump inhibitors, and some antiretroviral drugs can interfere with vitamin D metabolism or absorption, potentially leading to osteomalacia.
The time to reverse osteomalacia with treatment varies depending on the severity and underlying cause, but improvement in symptoms and bone mineralization can typically be observed within several months.
Raynaud’s disease, a condition affecting blood circulation, manifests in extreme sensitivity to cold temperatures or stress, causing the fingers, toes, and sometimes other extremities to turn white or blue and feel numb or cold. Named after the French physician Maurice Raynaud who first described it in 1862, this disorder affects millions worldwide, with various triggers and management strategies.
Understanding its nuances is crucial for those impacted. With proper knowledge, individuals can implement effective coping mechanisms and treatment plans to mitigate its effects and improve their quality of life. By delving into the intricacies of Raynaud’s disease, we can foster greater awareness and support for those navigating its challenges.
Table of Contents
Raynaud’s syndrome affects small blood vessels in fingers, toes, and other areas like the nose, lips, or ear lobes. Triggered by cold or stress, it causes spasms called vasospastic attacks.
During an attack, arterioles and capillaries tighten excessively, turning skin white and then blue due to oxygen deficiency. Skin may feel cold or numb, followed by redness or tingling as vessels relax. Attacks typically last 15 minutes.
There exist two classifications of Raynaud’s syndrome: primary and secondary.
According to a study conducted in 2020, the majority of individuals displaying these symptoms are diagnosed with primary Raynaud’s disorder, constituting 80-90 per cent of cases. This variant lacks a known cause and is considered idiopathic.
Secondary Raynaud’s syndrome is triggered by an underlying medical condition or certain medications. For instance, systemic sclerosis can induce Raynaud’s phenomenon and frequently serves as the initial indicator of the disease.
Individuals diagnosed with Raynaud’s may encounter symptoms ranging from moderate to severe.
Raynaud’s symptoms manifest in various ways, including:
Symptoms of Raynaud’s syndrome are episodic, lasting around 15 minutes typically, but can vary in duration. Triggers like cold weather often provoke episodes. Primary Raynaud’s syndrome tends to have milder symptoms, while secondary cases may involve more severe manifestations like skin ulcers.
You Can Also Read: Costochondritis: Symptoms, Causes, Diagnosis and Treatment
Primary Raynaud’s disease is characterised by the body’s response to cold or stress, restricting blood flow to the skin, and leading to symptoms. Factors impacting its occurrence include:
Secondary Raynaud’s links to medical conditions, medications, or habits like smoking, arthritis, and autoimmune diseases. Cold and stress are common triggers, urging attention to bodily signals.
Raynaud’s disease, characterised by vasospasm and reduced blood flow to extremities, poses potential complications, like:
Management involves avoiding triggers, keeping extremities warm, and seeking medical attention for severe symptoms. Treating underlying conditions is vital, particularly in secondary Raynaud’s, to mitigate complications.
To determine primary or secondary Raynaud’s syndrome, various diagnostic tests are available, such as:
These tests assist in diagnosing or ruling out underlying conditions contributing to Raynaud’s symptoms.
You Can Also Read: Prone to Frequent Lower Back Pain? 7 Things to Know About Ankylosing Spondylitis
There is no cure for primary or secondary Raynaud’s disease. Various therapies and modifications to your lifestyle, however, could assist in controlling your symptoms and lowering the frequency of episodes.
Raynaud’s disease poses unique challenges, yet with proper understanding and management, individuals can navigate its impact effectively. Increased awareness and support foster a better quality of life for sufferers. It is always advisable to seek medical help from an experienced rheumatologist. Timely care and help can ensure an appropriate diagnosis and treatment of your condition.
At the CK Birla Hospital, we ensure patients get holistic medical support which includes treatment in a compassionate environment. This patient-centric approach not only helps patients heal better but also ensures they are aware of the preventive measures as well. In case you need to consult a rheumatologist, reach out to us, or book a direct appointment at the CK Birla Hospital.
Raynaud’s disease can affect other body parts such as the nose, ears, nipples, and even internal organs like the lungs and heart in severe cases.
Raynaud’s disease can have a hereditary component, with a higher likelihood of occurrence in individuals with a family history of the condition.
In severe cases, Raynaud’s disease can lead to tissue damage, ulcers, and, rarely, gangrene in the affected fingers and toes, potentially resulting in permanent complications or amputation.
For managing Raynaud’s symptoms, consider a diet rich in omega-3 fatty acids, and antioxidants, and avoiding caffeine and alcohol. Keep warm and hydrated to improve blood circulation and reduce flare-ups.
Raynaud’s disease involves vasospasms triggered by cold or stress, causing reduced blood flow to extremities. Frostbite results from tissue freezing due to prolonged exposure to cold temperatures, leading to tissue damage.
Yes, stress can trigger Raynaud’s episodes by causing blood vessels to constrict, reducing blood flow to the extremities. Managing stress through relaxation techniques may help alleviate symptoms.
निश्चित रूप से, आपने अपने जीवन में कभी न कभी सिरदर्द की परेशानी का अनुभव किया होगा। क्या आपको वह तेज़ दर्द याद है जो आपकी दिनचर्या को बाधित करता है और बेहतर होता नहीं दिखता? अब उस दर्द की तीव्रता दोगुना हो जाता है और आपको जो सिरदर्द विकार होता है उसे माइग्रेन कहा जाता है। माइग्रेन का सिरदर्द दुनिया भर में लगभग 1 अरब लोगों को प्रभावित करता है। यह एक ऐसी स्थिति है जिसमें बार-बार दुर्बल करने वाला सिरदर्द होता है, जो मध्यम से गंभीर तक बढ़ जाता है। माइग्रेन रिसर्च फाउंडेशन के अनुसार, माइग्रेन सिरदर्द दुनिया में तीसरी सबसे आम बीमारी है। इतनी अधिक घटनाओं के बावजूद, माइग्रेन के लक्षण, कारण और उपचार के बारे में बहुत कम समझ है।
इस लेख में, प्रमुख आंतरिक चिकित्सा विशेषज्ञ डॉ तुषार तायल बताते हैं कि माइग्रेन क्या है और माइग्रेन के लक्षण क्या हैं।
Table of Contents
माइग्रेन एक बहुत ही सामान्य विकार है। यह एक न्यूरोलॉजिकल स्थिति है जो अत्यधिक दर्द का कारण बनती है और सिर के एक तरफ स्पंदन की अनुभूति कई घंटों या दिनों तक रह सकती है। माइग्रेन सिर्फ सिरदर्द से कहीं अधिक है क्योंकि यह आमतौर पर संवेदी गड़बड़ी (sensory disturbance) के बाद होता है। इन आभा विकारों में शामिल हैं:
यदि रोगी किसी भी प्रकार के शारीरिक परिश्रम में शामिल होता है तो दर्द बदतर हो जाता है। माइग्रेन 15 से 55 वर्ष की उम्र के लोगों को प्रभावित करता है।
माइग्रेन को दो मुख्य प्रकारों में वर्गीकृत किया जा सकता है जो इस बात पर निर्भर करता है कि रोगी संवेदी हानि या गड़बड़ी से पीड़ित है या नहीं। इन गड़बड़ियों को ऑरा के नाम से जाना जाता है। इसलिए, माइग्रेन के प्रकारों में शामिल हैं:
ये लक्षण कई रोगियों के लिए चेतावनी के रूप में कार्य करते हैं और माइग्रेन की शुरुआत का संकेत देते हैं। ऑरा की पहचान विभिन्न संवेदी गड़बड़ी से होती है जिनमें शामिल हैं:
जैसा कि नाम से पता चलता है, इस श्रेणी के अंतर्गत, रोगी को आभा संबंधी कोई हानि या संवेदना महसूस नहीं होती है। लगभग 70% से 90% लोग बिना किसी संवेदी गड़बड़ी या ऑरा के माइग्रेन का अनुभव करते हैं।
हालाँकि, बिना ऑरा वाले माइग्रेन में भी, एक व्यक्ति माइग्रेन के दौरे की शुरुआत या शुरुआत से गुजरता है और एक या दो दिन पहले लक्षणों का अनुभव करता है। इस अवस्था को प्रोड्रोम चरण के रूप में जाना जाता है।
ऑरा के आधार पर वर्गीकरण के अलावा, माइग्रेन के प्रकारों को भी विभाजित किया गया है। माइग्रेन के कुछ अन्य प्रकार हैं जो विशिष्ट सिंड्रोम और ट्रिगर से संबंधित हैं।
हालाँकि, लक्षणों के बारे में जानना महत्वपूर्ण है, लेकिन आपको अपनी स्थिति का स्वयं निदान नहीं करना चाहिए। यदि सिरदर्द माइग्रेन पैटर्न का अनुसरण करता है तो डॉक्टर से परामर्श करने का सुझाव दिया जाता है।
माइग्रेन के लक्षण उनके प्रकार और सिरदर्द की शुरुआत के चरण पर निर्भर करते हैं।
प्रोड्रोम चरण में सामान्य माइग्रेन लक्षणों में शामिल हैं:
ऑरा वाले माइग्रेन में, प्रोड्रोम चरण के बाद रोगी को कुछ संवेदी कठिनाइयों का अनुभव होता है। ऑरा के दौरान संवेदी अंग दृष्टि, गति, श्रवण, वाणी और/या संवेदना में हानि के साथ प्रभावित होते हैं। ऑरा के साथ सामान्य माइग्रेन सिरदर्द के लक्षणों में शामिल हैं:
कुख्यात माइग्रेन का दर्द इसके बाद होता है। इस चरण को आक्रमण चरण कहा जाता है। सभी चरणों में से सबसे गंभीर जिसके लिए माइग्रेन जाना जाता है। यह चरण घंटों या दिनों तक भी चल सकता है। इस चरण में दिखने वाले लक्षण हर व्यक्ति में अलग-अलग हो सकते हैं। हमले के चरण के कुछ सबसे आम माइग्रेन लक्षणों में शामिल हैं:
हमले के बाद, रोगी को आमतौर पर वह अनुभव होता है जिसे पोस्टड्रोम चरण कहा जाता है। इस चरण के दौरान मूड और भावनाओं में बदलाव का अनुभव होता है। यह उत्साहित और प्रसन्न से लेकर हल्के और सुस्त सिरदर्द के साथ थका हुआ और उदासीन हो सकता है।
इन चरणों की अवधि और डिग्री व्यक्ति दर व्यक्ति अलग-अलग होती है। एक चरण का छूट जाना असामान्य बात नहीं है और यह पूरी तरह से संभव है कि बिना किसी सिरदर्द के दौरा पड़ सकता है।
और अधिक पढ़े: डाउन सिंड्रोम क्या है: कारण, लक्षण, निदान और उपचार
माइग्रेन के कारणों को अभी तक पूरी तरह से समझा नहीं जा सका है। लेकिन जाहिर तौर पर इसका कारण आनुवंशिकी और पर्यावरणीय कारकों का मिश्रण है जो एक प्रमुख भूमिका निभाते हैं और इन्हें माइग्रेन का कारण माना जा सकता है।
मस्तिष्क की असामान्य गतिविधियों के कारण माइग्रेन का दर्द हो सकता है। यह तंत्रिकाओं के संचार के तरीके को प्रभावित करता है और रासायनिक असंतुलन का कारण बन सकता है। इस असंतुलन में सेरोटोनिन नामक मस्तिष्क रसायन में कमी शामिल है। आनुवंशिकी और एलर्जी भी एक बड़ी भूमिका निभाते प्रतीत होते हैं। उपरोक्त दो-तिहाई मामलों में, माइग्रेन पूरे परिवार में चलता है।
माइग्रेन ट्रिगर कोई भी पर्यावरणीय परिवर्तन, बाहरी उत्तेजना या शारीरिक क्रिया है जिसके परिणामस्वरूप माइग्रेन का सिरदर्द होता है। माइग्रेन अटैक के लिए कई ट्रिगर जिम्मेदार और कारण हैं जिनमें शामिल हैं:
महिलाओं में हार्मोनल बदलाव एक ट्रिगर की तरह काम करते हैं। मासिक धर्म, गर्भावस्था और/या रजोनिवृत्ति संक्रमण के कारण एस्ट्रोजन के स्तर में उतार-चढ़ाव तीव्र सिरदर्द को ट्रिगर करता है। मौखिक गर्भ निरोधकों और हार्मोन रिप्लेसमेंट थेरेपी जैसी हार्मोनल दवाओं के उपयोग के कारण यह खराब हो सकता है।
कुछ पेय पदार्थ, विशेष रूप से वे जिनमें अल्कोहल या कैफीन होता है, जैसे वाइन, कॉफी या एनर्जी ड्रिंक, पुरुषों और महिलाओं में माइग्रेन का कारण बन सकते हैं।
कुछ खाद्य पदार्थ माइग्रेन को ट्रिगर करने के लिए जाने जाते हैं जैसे पुराना पनीर और नमकीन प्रसंस्कृत भोजन। कुछ कृत्रिम मिठास का उपयोग करना या यहां तक कि भोजन छोड़ना भी माइग्रेन को ट्रिगर कर सकता है।
माइग्रेन का सबसे लोकप्रिय ट्रिगर तनाव है। घर या कार्यस्थल पर तनाव और तनाव व्यापक रूप से ज्ञात कारक हैं जो माइग्रेन का कारण बन सकते हैं।
मौखिक गर्भनिरोधक हार्मोनल असंतुलन और वैसोडिलेटर का कारण बन सकते हैं।
तीव्र शारीरिक परिश्रम में शामिल होने से सिरदर्द हो सकता है। इसलिए, नींद के पैटर्न में बदलाव हो सकता है या नींद गायब हो सकती है। कभी-कभी बहुत अधिक नींद और जेट लैग भी माइग्रेन का कारण बन सकते हैं।
इन सबके अलावा, तेज़ रोशनी जैसे सूरज की चमक, तेज़ आवाज़ या तेज़ गंध के संपर्क में आने से माइग्रेन हो सकता है।
माइग्रेन का कोई एक इलाज नहीं है और हर व्यक्ति का इलाज अलग-अलग हो सकता है। यदि आपको ऊपर बताए गए लक्षणों में से कोई भी लक्षण दिखाई देता है या यदि आपका सिरदर्द माइग्रेन पैटर्न के अनुसार होता है, तो डॉक्टर से मिलने का सुझाव दिया जाता है।
माइग्रेन का उपचार पूर्ण विकसित हमले को रोकने में मदद करता है। कभी-कभी माइग्रेन जीवनशैली और दैनिक आदतों में कुछ बदलावों से कम हो सकता है लेकिन कभी-कभी इसे ठीक करने के लिए सर्जरी की आवश्यकता हो सकती है। माइग्रेन से निपटने का सबसे अच्छा तरीका डॉक्टर से परामर्श करना और इसका निदान कराना है।
और अधिक पढ़े: मिर्गी क्या है – कारण, लक्षण और इलाज (Epilepsy, Seizure in Hindi)
चिकित्सा उपचार और जीवनशैली में संशोधन, संयुक्त रूप से माइग्रेन से छुटकारा पाने में मदद कर सकते हैं। जीवनशैली में कुछ बदलाव माइग्रेन में मदद कर सकते हैं जिनमें शामिल हैं:
आमतौर पर, उपचार के दौरान माइग्रेन की दवा की भी सलाह दी जाती है। किसी भी प्रकार की माइग्रेन की दवा शुरू करने से पहले हमेशा डॉक्टर से सलाह लें।
प्राथमिक अंतर यह है कि माइग्रेन एक सिरदर्द विकार है। यह सिरदर्द के कई प्रकारों में से एक है। आमतौर पर सिरदर्द सिर, चेहरे या गर्दन के ऊपरी हिस्से में महसूस होता है। जबकि माइग्रेन का सिरदर्द ज्यादातर सिर के एक तरफ महसूस होता है।
माइग्रेन का सिरदर्द एक थका देने वाला अनुभव हो सकता है और इसमें आपके जीवन के कई घंटे या दिन भी लग सकते हैं। माइग्रेन का प्रभावी इलाज पाने के लिए खुद को माइग्रेन के मूल सिद्धांतों के बारे में शिक्षित करना महत्वपूर्ण है।
हां, यह संभव है कि माइग्रेन का सिरदर्द अपने आप कम हो जाए। हालाँकि, यदि आपका सिरदर्द आपके दैनिक जीवन को गंभीर रूप से प्रभावित कर रहा है, तो आपको चिकित्सीय सहायता लेनी चाहिए।
माइग्रेन से छुटकारा पाने के लिए आप अपने सिर पर ठंडा या गर्म सेक लगा सकते हैं, अपने चारों ओर रोशनी कम कर सकते हैं और खूब पानी पी सकते हैं।
कुछ प्रसिद्ध खाद्य पदार्थ जो माइग्रेन से राहत दिलाने में मदद कर सकते हैं उनमें शकरकंद, गाजर, पालक, ब्राउन चावल आदि शामिल हैं।
आपको अपने माइग्रेन ट्रिगर्स जैसे कि पुरानी चीज, शराब और कैफीन की पहचान करनी चाहिए और उनसे बचना चाहिए।
Spinal Muscular Atrophy (SMA) is a rare genetic disorder affecting the motor neurons in the spinal cord, leading to muscle weakness and atrophy. Despite its low prevalence, SMA poses significant challenges to those diagnosed and their families.
This blog aims to shed light on the intricacies of SMA, including its causes, symptoms, available treatments, and ongoing research efforts to improve patient outcomes.
Table of Contents
An inherited neuromuscular condition known as spinal muscular atrophy (SMA). It weakens muscles as it targets motor neurons in the spinal cord, which control muscle movement. Without these neurons, muscles receive no signals for movement. This leads to muscle atrophy, where muscles shrink and weaken due to inactivity.
The four main forms of spinal muscular atrophy are as follows:
You Can Also Read: Common spine issues that can affect anyone and how to prevent them
Spinal Muscular Atrophy (SMA) presents varying symptoms, and severity depending on the age of onset:
In infants, symptoms are severe and potentially life-threatening, such as:
SMA also includes:
Management involves swallowing therapy, mobility aids, and possibly feeding tubes, to address symptoms and enhance quality of life.
SMA is caused by a deficiency in the SMN1 gene, leading to insufficient SMN protein production vital for motor neuron health. Without enough SMN protein, motor neurons deteriorate, impairing voluntary movement control, especially in the head, neck, arms, and legs.
Individuals possess SMN2 genes, which can partially compensate for SMN1 deficiency, with up to eight copies per person. More SMN2 copies often correlate with milder SMA symptoms due to increased SMN protein production.
Occasionally, SMA stems from mutations in genes other than SMN1 (non-chromosome 5), although this is rare.
Some symptoms of Spinal Muscular Atrophy (SMA) mimic those seen in neuromuscular disorders such as muscular dystrophy. Healthcare providers conduct physical exams and review medical histories to ascertain the underlying cause of symptoms. The diagnostic tests for SMA are:
The prenatal tests for SMA include:
You Can Also Read: Caring for Your Spine: Understanding Degenerative Disc Disease
SMA lacks a cure. Treatments vary based on SMA type and symptoms. Physical therapy, occupational therapy, and assistive devices like braces, crutches, walkers, and wheelchairs aid many SMA patients.
Disease-modifying therapy like Nusinersen stimulates SMN protein production, administered via spinal canal injection. Risdaplam, taken orally, aids adults and children older than two months.
Gene replacement therapy benefits infants under two through a one-time IV infusion of onasemnogene abeparvovec-xioi, replacing a faulty SMN1 gene with a functional one.
Throughout their condition, individuals with SMA undergo a gradual decline in muscle strength and coordination. This progression may lead to various complications, such as:
Inheritance of SMA is a genetic phenomenon. Should either you or your partner possess the mutated gene responsible for SMA, consulting a genetic counsellor can provide insights into the likelihood of your child inheriting SMA or becoming a carrier.
Before conception, steps can be taken to reduce the risk of passing on SMA. Preimplantation genetic diagnosis (PGD) identifies embryos without the mutated gene, ensuring that during in vitro fertilization (IVF), only healthy embryos are implanted. This method ensures that your child will inherit two healthy SMN1 genes, preventing SMA.
Spinal muscular atrophy poses significant challenges, but advancements in research, treatment, and support offer hope. Through continued efforts, we strive for improved outcomes and a brighter future. It is always advisable to seek medical help from an experienced neurologist. Timely care and help can ensure an appropriate diagnosis and treatment of your condition.
At the CK Birla Hospital, we ensure patients get holistic medical support which includes treatment in a compassionate environment. This patient-centric approach not only helps patients heal better but also ensures they are aware of the preventive measures as well. In case you need to Consult a Neurologist, reach out to us, or book a direct appointment at the CK Birla Hospital.
The life expectancy of someone with Spinal Muscular Atrophy (SMA) varies greatly depending on the type and severity of the condition, but it can range from infancy to adulthood.
Yes, although it’s less common, adults can develop SMA due to genetic mutations or late-onset presentations. Symptoms may vary in severity and can appear later in life.
If one parent is a carrier of the SMA gene mutation, each child has a 50% chance of inheriting the mutated gene, which could lead to SMA if both parents pass it on.
SMA (Spinal Muscular Atrophy) weakens respiratory muscles, leading to difficulty breathing, reduced lung capacity, and increased susceptibility to respiratory infections, impacting overall respiratory function and potentially causing respiratory failure.
Shingles, caused by the varicella-zoster virus, is a painful rash that typically appears on one side of the body. While often associated with older adults, it can affect individuals of any age who have had chickenpox.
Understanding its symptoms, risk factors, and available treatments is crucial for managing this condition effectively. Explore this blog to gain insights into shingles and its impact on health.
Table of Contents
Shingles (herpes zoster) is a painful rash caused by the varicella-zoster virus, which also causes chickenpox. The rash typically appears as a band of blisters on one part of the body. After childhood chickenpox, the virus remains dormant in the body. In adulthood, it can reactivate as shingles.
The first symptoms of shingles often start with pain and burning, typically affecting one side of the body in a specific skin area known as a dermatome. A subsequent rash, though not always red, may appear dark pink, dark brown, or purplish, depending on skin tone.
The characteristics of a shingles rash outlined by the National Institute on Aging (NIA) are:
Additional symptoms per the American Academy of Dermatology may include:
Other complications (which are rare):
Shingles can manifest in various areas, such as:
You Can Also Read: Types of Skin Problems & their Solutions
Shingles arise from the varicella-zoster virus, the same virus responsible for chickenpox. If you’ve had chickenpox previously, shingles can occur when this virus becomes active again in your system.
The exact cause of why shingles affect certain individuals remains uncertain. Its prevalence tends to be higher among older adults due to reduced immunity to infections.
Potential factors that may increase the risk of shingles include:
Shingles are typically diagnosed by doctors through a thorough examination of your rashes and blisters, accompanied by inquiries into your medical background.
Occasionally, if necessary, your physician might require a skin sample or fluid from the blisters for testing. This process entails the use of a sterile swab to gather tissue or fluid, which is then sent to a medical lab to validate the virus’s presence.
There is no cure for shingles, but various treatments help manage symptoms, such as:
These drugs can alleviate discomfort and shorten symptom duration if taken within 72 hours of the first sign of shingles. They might lessen the chance of developing postherpetic neuralgia as well.
These medications can provide relief from pain associated with shingles.
You Can Also Read: Suffering From Tinea Cruris Or Jock Itch (Groin Ringworm)
While shingles can cause considerable discomfort, it’s essential to remain vigilant about potential complications, like:
Vaccination can prevent severe shingles symptoms. Two doses of the chickenpox vaccination are required for children.
Adults without prior chickenpox should also receive it. While not guaranteed, the vaccine prevents chickenpox in 9 out of 10 cases.
Adults over 50 should get the shingles vaccine to avoid severe symptoms. Consult your doctor to determine if you need the shingles vaccine.
Shingles can be a painful and debilitating condition, but with proper understanding, prevention, and medical care, individuals can effectively manage and overcome its challenges for a healthier future. It is always advisable to seek medical help from an experienced dermatologist. Timely care and help can ensure an appropriate diagnosis and treatment of your condition.
At the CK Birla Hospital, we ensure patients get holistic medical support which includes treatment in a compassionate environment. This patient-centric approach not only helps patients heal better but also ensures they are aware of the preventive measures as well. In case you need to consult a dermatologist, reach out to us, at the CK Birla Hospital.
Shingles can indeed recur several times. Although uncommon, individuals who have had shingles can experience a recurrence due to the reactivation of the varicella-zoster virus.
Shingles can be contagious, but it only spreads through direct contact with the rash during the blister phase. It can transmit the varicella-zoster virus, causing chickenpox in susceptible individuals.
Long-term effects of shingles may include postherpetic neuralgia (chronic pain), scarring, changes in vision or hearing if the eyes or ears are affected, and in rare cases, neurological complications.
Shingles can affect internal organs if the virus spreads to them. This may lead to complications such as pneumonia, encephalitis, or inflammation of other internal organs.
Shingles and chickenpox are caused by the same virus, varicella-zoster, but present differently. Chickenpox is a widespread rash, while shingles is a localised, painful rash along a nerve pathway.
Shingles typically last 2 to 4 weeks. However, complications like postherpetic neuralgia can prolong symptoms. Early treatment can help shorten the duration and reduce the severity of the illness.
Yes, stress can trigger shingles outbreaks by weakening the immune system, allowing the varicella-zoster virus to reactivate. Managing stress through relaxation techniques and healthy lifestyle habits may help prevent recurrences.
In today’s dynamic business landscape, where competition is fierce and talent is the key differentiator, organizations must continuously evolve to stay ahead. At the CK Birla Hospital, we recognize that our greatest asset is our people, and fostering a workplace culture where employees thrive is paramount to our success. That’s why earning the prestigious Great Place To Work (GPTW) certification isn’t just a milestone; it’s a strategic imperative that positions us for accelerated growth and sustainable success.
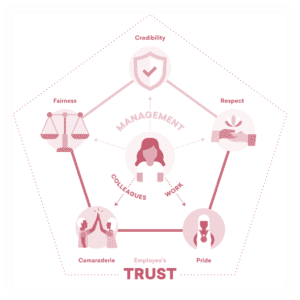
GPTW Trust Framework
The CK Birla Hospital stands out as a great place to work for several compelling reasons, each rooted in our unwavering commitment to fostering a culture of excellence, empathy, and empowerment. Here are some key factors that contribute to making CK Birla Hospital a great workplace:
At the heart of CK Birla Hospital is a deep appreciation for our people. We recognize that our employees are our most valuable asset, and we prioritize their well-being, growth, and development above all else. Our people-centric culture is reflected in every aspect of our organization, from our inclusive leadership style to our transparent communication practices.
We go above and beyond to ensure that our employees feel supported, valued, and empowered. From comprehensive health and wellness programs to flexible work arrangements and employee assistance programs, we prioritize the physical, mental, and emotional well-being of our workforce.
At the CK Birla Hospital, we believe in investing in our employees’ growth and development. We provide ample opportunities for learning, training, and career advancement, enabling our employees to realize their full potential and achieve their professional goals.
Collaboration is at the core of our organizational DNA. We foster a culture of teamwork, respect, and inclusivity, where every voice is heard and every contribution is valued. Our diverse workforce brings together individuals from different backgrounds, perspectives, and experiences, enriching our collective learning and driving innovation.
Our leadership team leads by example, embodying our core values of integrity, accountability, and empathy. They provide clear direction, guidance, and support, empowering employees to take ownership of their work and contribute meaningfully to our shared goals and objectives.
Whether through formal recognition programs, employee appreciation events, or personalized acknowledgements, we ensure that our employees feel valued, appreciated, and motivated to continue delivering their best.
We prioritize open, honest, and transparent communication at all levels of the organization. We believe in keeping our employees informed and engaged, fostering a culture of trust, collaboration, and accountability.
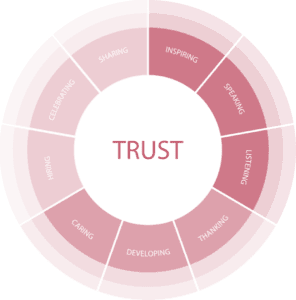
GPTW Trust Framework
As we embark on this transformative journey, we’re poised to leverage our GPTW certification as a springboard for organizational advancement. Getting certified by GPTW implies that our operations and policies are aligned with industry best practices. These are:
By showcasing our commitment to employee well-being and professional development, we’re able to attract high-calibre talent who are aligned with our values and vision for the future.
Engaged employees are the driving force behind organizational success. By prioritizing factors such as fairness, transparency, and inclusivity, we empower our employees to bring their best selves to work each day, driving productivity, innovation, and ultimately, organizational growth.
Employee satisfaction directly correlates with customer satisfaction. As satisfied and engaged employees deliver superior service and care to our patients, we’re able to enhance customer satisfaction and loyalty.
We unlock innovation by empowering employees to share ideas, experiment, and challenge the norm. This positions us for long-term success in a competitive market.
By showcasing our commitment to employee well-being, integrity, and excellence, we’re able to attract patients, partners, and investors who share our values and support our mission for growth and impact.
A positive workplace culture directly impacts operational efficiency and effectiveness. By investing in our employees’ development, well-being, and job satisfaction, we’re able to enhance employee morale, reduce turnover, and drive efficiencies that contribute to bottom-line growth and sustainability.
Continuous learning and development are essential for organizational growth and resilience. By investing in training, mentorship, and career development programs, we’re able to empower our employees to reach their full potential, driving individual and organizational growth in tandem.
What makes the CK Birla Hospital a great place to work is our unwavering commitment to our people, our values, and our shared vision for excellence. By prioritizing employee well-being, fostering a collaborative and inclusive environment, providing opportunities for growth and advancement, and embodying strong leadership and vision, we create a workplace where every individual can thrive, contribute, and make a meaningful difference.
डाउन सिंड्रोम एक आनुवंशिक विकार है जिससे पीड़ित व्यक्ति के पास एक अतिरिक्त गुणसूत्र (क्रोमोसोम) या गुणसूत्र का एक अतिरिक्त टुकड़ा होता है। यह विभिन्न शारीरिक और संज्ञानात्मक (कॉग्निटिव) समस्याओं को जन्म देता है, जिसमें विकासा में देरी, बौद्धिक अक्षमताएं, चेहरे की विशिष्ट विशेषताएं जैसे कि तिरछी आंखें और एक सपाट नाक एवं हृदय दोष और थायराइड की समस्या आदि शामिल हैं।
डाउन सिंड्रोम वाले व्यक्तियों को चुनौतियों का सामना करना पड़ सकता है, कई लोग उचित समर्थन और संसाधनों के साथ पूर्ण जीवन जीते हैं। प्रारंभिक हस्तक्षेप कार्यक्रम और समावेशी (इन्क्लूसिव) शिक्षा उनके जीवन की गुणवत्ता में सुधार करने में मदद करती है और उन्हें समाज में सकारात्मक योगदान देने में सक्षम बनाती है।
Table of Contents
डाउन सिंड्रोम को मुख्य रूप से तीन प्राथमिक प्रकारों में बांटा गया है जिसमें निम्न शामिल हैं:
यह सबसे आम प्रकार है, जो लगभग 95% मामलों में होता है। यह क्रोमोसोम 21 की एक अतिरिक्त टुकड़ा के कारण होता है, जिससे प्रत्येक कोशिका में सामान्य दो की बजाय कुल तीन टुकड़े बन जाते हैं। ट्राइसॉमी 21 आमतौर पर माता-पिता में प्रजनन कोशिकाओं के निर्माण के दौरान उत्पन्न होता है, जिसके परिणामस्वरूप निषेचित अंडे में एक अतिरिक्त गुणसूत्र 21 बनता है।
लगभग 3% मामलों में यह प्रकार होता है। यह तब होता है जब कोशिका विभाजन के दौरान क्रोमोसोम 21 का एक हिस्सा टूट जाता है और दूसरे क्रोमोसोम, अक्सर क्रोमोसोम 14 से जुड़ जाता है। हालांकि, क्रोमोसोम की कुल संख्या 46 रहती है, अतिरिक्त आनुवंशिक मटेरियल डाउन सिंड्रोम की विशिष्ट विशेषताओं का कारण बनती है।
यह एक दुर्लभ रूप है, जो लगभग 2% मामलों में होता है। मोज़ेक डाउन सिंड्रोम वाले व्यक्तियों में कोशिकाओं का मिश्रण होता है, कुछ में क्रोमोसोम 21 की विशिष्ट दो टुकड़े होते हैं और अन्य में तीन। इस मोज़ेक पैटर्न की उपस्थिति निषेचन के बाद कोशिका विभाजन में त्रुटियों के परिणामस्वरूप होती है, जिससे डाउन सिंड्रोम से जुड़ी शारीरिक और बौद्धिक विशेषताओं की अलग-अलग डिग्री होती है।
और अधिक पढ़े: क्या क्लबफुट का स्थायी इलाज संभव है?
डाउन सिंड्रोम मुख्य रूप से आनुवंशिक विसंगतियों से उत्पन्न होता है। सबसे आम कारण ट्राइसॉमी 21 है, जो लगभग 95% मामलों में होता है, जहां गुणसूत्र 21 की एक अतिरिक्त प्रतिलिपि/टुकड़ा/कॉपी होती है। यह अतिरिक्त आनुवंशिक मटेरियल विशिष्ट विकास को बाधित करती है और डाउन सिंड्रोम की विशिष्ट विशेषताओं की ओर ले जाती है।
ट्रांसलोकेशन डाउन सिंड्रोम, लगभग 3% मामलों में, क्रोमोसोम 21 और दूसरे क्रोमोसोम के बीच आनुवंशिक मटेरियल के पुनर्व्यवस्था के परिणामस्वरूप होता है। जबकि गुणसूत्रों की कुल संख्या सामान्य रहती है, गुणसूत्र 21 से अतिरिक्त आनुवंशिक सामग्री सामान्य सेलुलर कार्यों को बाधित करती है।
लगभग 2% मामलों में होने वाला मोज़ेक डाउन सिंड्रोम, निषेचन के बाद कोशिका विभाजन के दौरान त्रुटियों से उत्पन्न होता है। इसके परिणामस्वरूप कुछ कोशिकाओं में गुणसूत्र 21 की सामान्य दो टुकड़े/प्रतियां होती हैं, जबकि अन्य में तीन होती हैं। मोज़ेक पैटर्न डाउन सिंड्रोम से जुड़े लक्षणों और चुनौतियों की अलग-अलग डिग्री की ओर ले जाता है।
सभी प्रकारों में, डाउन सिंड्रोम की ओर ले जाने वाली आनुवंशिक विसंगति का विशिष्ट कारण हमेशा स्पष्ट नहीं होता है, लेकिन उन्नत मातृ आयु एक ज्ञात जोखिम कारक है, विशेष रूप से ट्राइसॉमी 21 के लिए। हालाँकि, यह स्थिति किसी भी उम्र की महिलाओं की गर्भावस्था में हो सकती है।
डाउन सिंड्रोम शारीरिक, विकासात्मक और संज्ञानात्मक लक्षणों की एक श्रृंखला प्रस्तुत करता है। डाउन सिंड्रोम वाले व्यक्ति अपनी क्षमताओं और विशेषताओं में व्यापक रूप से भिन्न हो सकते हैं, कुछ सामान्य लक्षणों में निम्न शामिल हैं:
इन सबके अलावा, डाउन सिंड्रोम वाले व्यक्तियों में थायरॉयड विकार, मोटापा, गैस्ट्रोइंटेस्टाइनल समस्याएं और ल्यूकेमिया जैसी स्वास्थ्य समस्याएं विकसित होने का खतरा अधिक होता है।
और अधिक पढ़े: सेरेब्रल पाल्सी: कारण, लक्षण और इलाज
डाउन सिंड्रोम का निदान आमतौर पर गैर-इनवेसिव प्रीनेटल परीक्षण (एनआईपीटी), अल्ट्रासाउंड या एमनियोसेंटेसिस जैसे स्क्रीनिंग परीक्षणों के माध्यम से किया जाता है, जो भ्रूण की आनुवंशिक मटेरियल का विश्लेषण करते हैं या भौतिक मार्करों का आकलन करते हैं। जन्म के बाद, क्रोमोसोमल कैरियोटाइप विश्लेषण जैसे आनुवंशिक परीक्षण के माध्यम से निदान की पुष्टि की जाती है, जो अतिरिक्त क्रोमोसोम 21 की उपस्थिति के लिए कोशिकाओं की जांच करता है। प्रारंभिक निदान डाउन सिंड्रोम वाले व्यक्तियों और उनके परिवारों का समर्थन करने के लिए समय पर उचित चिकित्सा और विकासात्मक हस्तक्षेप में मदद करता है।
हालांकि, डाउन सिंड्रोम का कोई इलाज नहीं है, लेकिन इस स्थिति वाले व्यक्तियों को उनकी विशिष्ट आवश्यकताओं को पूरा करने के उद्देश्य से कई उपचारों और हस्तक्षेपों से लाभ होता है। प्रारंभिक हस्तक्षेप कार्यक्रम विकास का समर्थन करने और कौशल बढ़ाने के लिए शारीरिक, व्यावसायिक और भाषण चिकित्सा जैसी चिकित्साएँ प्रदान करते हैं। व्यक्तिगत शिक्षण शैलियों के अनुरूप शैक्षिक कार्यक्रम शैक्षणिक और सामाजिक विकास को बढ़ावा देने में मदद करते हैं।
चिकित्सा प्रबंधन हृदय दोष, दृष्टि और सुनने की समस्याएं, थायरॉइड डिसफंक्शन और ल्यूकेमिया जैसे संबंधित स्वास्थ्य समस्याओं को संबोधित करने पर केंद्रित है। परामर्श और सामाजिक सहायता नेटवर्क सहित सहायक सेवाएँ, डाउन सिंड्रोम से जुड़ी चुनौतियों से निपटने में परिवारों की सहायता करती हैं और समुदायों के भीतर समावेश और स्वीकृति को बढ़ावा देती हैं।
जैसे ही डाउन सिंड्रोम वाले व्यक्ति वयस्कता की ओर बढ़ते हैं, व्यावसायिक प्रशिक्षण और रोजगार सहायता उन्हें स्वतंत्रता प्राप्त करने और समाज में सार्थक योगदान देने में सक्षम बनाती है। नियमित स्वास्थ्य निगरानी और विशेष सेवाओं तक पहुंच सहित व्यापक देखभाल, यह सुनिश्चित करती है कि डाउन सिंड्रोम वाले व्यक्ति पूर्ण जीवन जी सकते हैं और अपनी पूरी क्षमता तक पहुंच सकते हैं।
In the realm of women’s health, discussions about vaginal discharge can be both sensitive and crucial. One such type that often raises concern is cottage cheese-like discharge, which may indicate various underlying conditions.
Understanding its causes, symptoms, and potential treatments is essential for maintaining vaginal health and seeking timely medical advice when necessary. Let’s delve into this topic to shed light on what cottage cheese vaginal discharge signifies.
Table of Contents
Cottage cheese vaginal discharge is thick, white, and curd-like, resembling cottage cheese. It’s often a symptom of a yeast infection caused by Candida overgrowth in the vagina. Other symptoms may include itching, burning, and irritation. It’s crucial to consult a healthcare professional for proper diagnosis and treatment, as other conditions may present with similar discharge.
Symptoms of “cottage cheese” vaginal discharge, often indicative of a yeast infection, include:
See a medical professional for a precise diagnosis and the best course of action.
The occurrence of cottage cheese discharge can be linked to a variety of factors and conditions, such as:
You Can Also Read: Spotting Before Menstruation: Reasons and When to Seek Help
Diagnosis of cottage cheese vaginal discharge typically involves a combination of medical history review, physical examination, and laboratory tests, such as:
Seek medical evaluation for accurate diagnosis and tailored treatment if experiencing symptoms akin to cottage cheese-like discharge. Consulting a healthcare professional ensures proper management through comprehensive assessment.
Cottage cheese-like discharge often signals a yeast infection from Candida albicans overgrowth. Treatment involves antifungal meds, OTC or prescribed. Common antifungal treatments include:
Consult a healthcare provider for an accurate diagnosis before starting treatment, as other vaginal infections may have similar symptoms. Follow medication instructions carefully and complete the full course. Seek further evaluation if symptoms persist or worsen.
Natural remedies for cottage cheese-like vaginal discharge, often a sign of a yeast infection, include:
Consult a healthcare provider for accurate diagnosis and treatment, especially for recurrent or worsening symptoms.
You Can Also Read: Suffering From Vaginal Yeast Infection In Summer? Know Its Treatment & Prevention
Seek a healthcare provider’s help for cottage cheese-like vaginal discharge in the following situations:
Overall, if unsure, consulting a healthcare provider is advisable for proper diagnosis and personalised treatment.
While cottage cheese-like vaginal discharge can be a sign of a yeast infection, it’s crucial not to self-diagnose. Maintaining good hygiene practices and a balanced diet can help prevent such infections and ensure your reproductive health and overall well-being. It is always advisable to seek medical help from an experienced gynaecologist. Timely care and help can ensure an appropriate diagnosis and treatment of your condition.
At the CK Birla Hospital, we ensure patients get holistic medical support which includes treatment in a compassionate environment. This patient-centric approach not only helps patients heal better but also ensures they are aware of the preventive measures as well. In case you need to consult a gynaecologist, reach out to us, or book a direct appointment at the CK Birla Hospital.
Yeast infections are typically not sexually transmitted, but sexual activity can increase risk factors. However, partners can pass yeast to each other through sexual contact in rare cases.
Yeast infections are caused by Candida overgrowth, leading to itching and thick discharge, while bacterial vaginosis results from an imbalance of vaginal bacteria, causing a fishy odour and thin discharge.
Yes, over-the-counter antifungal medications are available without a prescription for treating yeast infections. However, it’s essential to follow instructions carefully and consult a healthcare provider if symptoms persist or worsen.
Maintaining a balanced diet low in sugar and refined carbohydrates, and high in probiotics and fibre, can help prevent yeast infections by promoting healthy vaginal flora and immune function.
Yes, stress can weaken the immune system and disrupt the balance of microorganisms in the body, potentially increasing susceptibility to yeast infections. Stress management may help reduce this risk.
Recurrent yeast infections can lead to discomfort, and psychological distress, and potentially compromise fertility. In rare cases, they may indicate underlying health conditions warranting medical attention.
A breast cancer diagnosis can feel like a heavy blow, shrouded in stigma and fear. For many women, the prospect of a subsequent mastectomy can deepen feelings of despair and uncertainty. However, amidst the darkness, there’s a glimmer of hope: the power of early detection and advancements in surgical technology, particularly robotic-assisted surgery. The latest innovation in onco-surgeries, robotic surgery is revolutionising breast cancer treatment, offering patients a lifeline of hope, confidence, and preservation.
Table of Contents
Breast cancer remains one of the most stigmatised diseases, often overshadowed by misconceptions and fear. The fear of judgement and the unknown can prevent women from seeking timely medical attention, delaying diagnosis and treatment. However, breaking the silence and fostering open conversations about breast health is crucial in dispelling myths and empowering women to prioritise their well-being.
Often breast cancer is so advanced that there is no option but to remove the breast tissue completely by performing a mastectomy. The prospect of a mastectomy can plunge breast cancer patients into a whirlwind of emotions, from grief and anger to anxiety and uncertainty. The loss of a breast for a woman is not merely physical but deeply emotional, challenging one’s sense of identity and femininity. Healthcare providers need to offer compassionate support and guidance, helping patients navigate the emotional turmoil and make informed decisions about their treatment journey.
Amidst the challenges of a breast cancer diagnosis, maintaining motivation and resilience is paramount. Empowering patients with knowledge about their treatment options and the importance of early detection can instil a sense of agency and control. Additionally, providing access to support groups, counselling services, and holistic care can bolster patients’ emotional well-being and foster a sense of community and camaraderie.
Early detection is the cornerstone of successful breast cancer treatment, offering the best chance of preserving the breast and achieving optimal outcomes. Regular screening mammograms and self-breast exams empower women to detect abnormalities early, allowing for timely intervention and breast conservation.
By prioritising proactive breast health measures, women can take control of their health and well-being, potentially avoiding the need for more extensive surgical interventions. A host of new and alternative treatment options are helping oncologists tackle breast cancer better.
Take, for instance, a 28-year-old mother of an infant who presented with advanced breast cancer. Treated with a combination of neoadjuvant chemotherapy and immunotherapy, she underwent robotic-assisted functional breast preservation surgery. The procedure involved the removal of the affected portion of breast tissue while preserving the original breast skin and reconstructing with tissue from the back, all through a single incision. The outcome? Precision, minimal scarring, and remarkable aesthetics, with the patient now cancer-free and with a sensate breast that feels the same as it did before cancer.
In another case, a 60-year-old woman with nipple retraction underwent robotic-assisted surgery with the aid of indocyanine green (ICG) navigation technology. The team successfully identified and excised a suspicious breast lesion, providing swift clarity on malignancy. This technology, employed in 90% of recent breast cancer surgeries, enables accurate diagnosis and facilitates breast conservation surgeries with oncoplasty, preserving both life and confidence.
Enter robotic-assisted surgery, a groundbreaking approach that is revolutionising the field of breast cancer treatment. At the CK Birla Hospital Gurgaon, Dr. Mandeep Malhotra is leading the way in robotic-assisted breast cancer surgery, offering patients unparalleled precision, minimal scarring, and enhanced aesthetic outcomes. By harnessing the power of robotics, Dr. Malhotra and his team can approach delicate breast surgeries with unmatched accuracy and efficiency, minimising trauma to surrounding tissues and preserving vital aspects of the breast.
Breast cancer may cast a shadow of uncertainty, but with advancements in surgical technology and a compassionate approach to care, there is hope. At the CK Birla Hospital( Gurgaon, we’re proud to lead the charge in robotic-assisted breast surgery, empowering patients with personalised, precision-driven care that preserves both life and dignity. “Cancer does not discriminate. Neither is it predictable. But as oncologists, our goal is not only to increase survival but also prioritise the patient’s quality of life.” Dr Mandeep S Malhotra, Surgical and Molecular Oncologist.
Robotic-assisted surgery offers a beacon of light, guiding breast cancer patients toward preservation, confidence, and survivorship. Together, let’s rewrite the narrative of breast cancer treatment, one robotic arm at a time.