Filter :
There are some things in life that we tend to ignore unless we find something bothersome about them. For instance, urine. When was the last time you thought of something like urination? Our guess: when you felt pain or discomfort like a burning sensation when urinating.
Most of us can relate to the burning sensation after urinating. However common, it is a serious health concern that we must not ignore. In this article, Dr Shalabh Agrawal, the best urologist in Gurgaon, talks about the reason for pain during and after urination.
Table of Contents
Here are some of the common symptoms of dysuria in women and men.
Dysuria occurs when the urinary tract suffers from inflammation, injury or infections. There is a wide range of conditions that cause pain during urination by harming the urinary system.
A burning sensation when urinating is an indicator of some other health condition. If this symptom is ignored, you cannot get proper treatment for the root cause.
Pain during urination can lead to various complications such as chronic pain, sepsis (a blood infection), infertility and spread of numerous other infections.
While mild burning or discomfort during urination may sometimes resolve on its own, certain warning signs should never be ignored. These symptoms may indicate that the problem is more serious and requires urgent medical care:
Your healthcare provider will do preliminary investigations to find the cause of painful urination. He/she will discuss your personal medical history and symptoms. It is helpful to track symptoms if the burning and pain when urinating has lasted for a long time.
Your urologist or gynaecologist will perform some basic diagnostic tests. You can expect to have blood tests, urine tests, ultrasound scans and X-rays. You may be indicated for additional tests depending upon your overall health.
The diagnosis is drawn to figure out the dysuria causes.
The treatment module is dependent upon the reason behind dysuria. The accuracy of the diagnosis can help your doctor decide which treatment method to offer.
1. Urinary Tract Infections (UTIs)
2. Vaginitis
Vaginitis is inflammation of the vagina due to infections or an imbalance of natural bacteria/yeast. Treatment depends on the type:
3. Sexually Transmitted Infections (STIs)
STIs that cause burning urination are treated with targeted medicines:
4. Interstitial Cystitis (Bladder Pain Syndrome)
This is a chronic condition where no infection is found but bladder pain and frequent urination persist. Management includes:
5. Menopause-Related Symptoms
In postmenopausal women, reduced oestrogen levels can cause thinning and dryness of the vaginal and urethral tissues, leading to burning or pain while urinating.
Treatment may include oestrogen therapy:
Note: The above is a general overview of dysuria treatment. Do not self-medicate. Your doctor will prescribe you the right treatment plan as per your unique health condition.
It is highly normal to feel a burning sensation when urinating once in a while. If you continue to experience painful urination along with other symptoms, then you should seek clinical care.
You can book an appointment with Dr Shalabh Agrawal, a senior urologist at the CK Birla Hospital, to learn more about the health of the urinary tract.
Ques: How can I prevent the burning sensation when urinating?
Ans: You can prevent burning sensation when urinating (dysuria) by drinking plenty of water, increasing your intake of Vitamin C and passing urine whenever the need arises.
Ques: What complications can arise if I don’t address dysuria?
Ans: Untreated dysuria can further cause chronic pain, sepsis (a blood infection), infertility and spread of numerous other infections.
Ques: When should I seek medical help for burning sensation when urinating?
Ans: You should consult a medical expert if you see blood in the urine or have a high-grade fever along with persistent painful urination.
Ques: How can I avoid UTI?
Ans: You can avoid UTI by staying hydrated, restricting your consumption of caffeine, maintaining hygiene and completely emptying your bladder every time you pass urine.
Most Indians have an extraordinary liking for street foods. The spicy tangy flavourful snacks served by vendors have a special place in our hearts. When you have such appetizing options, you will not be a fan of bland food. However, there is one thing worse than eating bland and boring meals – food poisoning. This article explores what is food poisoning along with its symptoms, causes and treatment.
Food borne illnesses are highly common in India with a prevalence of nearly 13% at a household level. Food poisoning symptoms are seldom overlooked as they impact your levels of comfort and everyday tasks. Let us begin by understanding the meaning of food poisoning.
Table of Contents
Food poisoning is a common foodborne illness. It is caused when you consume contaminated or spoiled food items. Contamination happens when food items get exposed to infectious organisms such as viruses, bacteria and parasites.
Mostly, these organisms are killed when food is cleaned and cooked properly. These infectious organisms are able to access your digestive system when you consume uncooked or raw eatables.
Food poisoning is a common condition that can impact anyone, irrespective of their age and gender.
There is a wide range of ailments that target your stomach and digestion. It can be slightly difficult to distinguish them from one other. For instance, the symptoms of stomach flu and food poisoning often overlap. Stomach flu, however, is caused by viruses. Due to this overlapping, it is significant to learn about the signs and symptoms of food poisoning.
Common signs and symptoms of food poisoning include:
You should ensure to consult a healthcare provider if you experience any of the above-given symptoms. There are several life-threatening food poisoning symptoms that require immediate medical intervention.
See a healthcare provider immediately if:
Primarily, food poisoning is caused by the consumption of toxic and contaminated food. Three types of organisms are accountable for this illness – bacteria, parasites and viruses.
Almost all food products can be targeted by these organisms. The contamination of food is possible at any stage starting from its production till cooking. These infectious agents are present at several surfaces and can transfer from one surface to another.
While everyone is vulnerable to being affected by food poisoning, some people are at a higher risk than others. The groups of people at an increased risk for this illness include older adults, infants, young children, pregnant women and chronically ill people.
Food poisoning cure is its effective and early treatment. Several treatment methods are available for the treatment of food poisoning. However, a precise diagnosis is the first step towards a food poisoning cure.
Your doctor will ask about your medical history. A detailed discussion on the symptoms and their length is mostly enough for healthcare providers to draw a diagnosis.
You can expect to have a physical health checkup. Your doctor will ask you about the food items you must have consumed recently to find out the possible source of contamination. Your healthcare provider may indicate a variety of tests including blood workup, stool sample culture test and more.
Your doctor will offer a relevant treatment method based on your diagnosis and the source of food poisoning.
Since food poisoning can trigger diarrhea and vomiting, you may lose excess body fluids. Your doctor will ask you to drink as many fluids as possible. He/she may prescribe consuming electrolytes to compensate for the loss of fluids. Nevertheless, some foods and beverages such as alcohol, caffeine and spicy foods should be restricted.
You will also be asked to monitor your meals. Avoid eating food products that may trigger your symptoms further. You will be asked to eat bland and easy to digest foods.
Additionally, your doctor will prescribe relevant medicines to alleviate your symptoms and offer instant relief. Mostly, sufficient rest and careful measures are enough to resolve food poisoning.
A proactive and healthy lifestyle can help you in the prevention of food poisoning. Here are some expert-approved home remedies you should implement to avoid this illness:
A severe and persistent case of food poisoning can further worsen your health. The most common complications of this illness are:
It is not very complex to grasp the idea of what is food poisoning. To put it briefly, food poisoning is a common digestive illness caused by viruses, bacteria or parasites. You should focus on cleaning yourself and your surroundings clean to avoid the transfer of germs.
Book an appointment at the CK Birla Hospital to know more about food poisoning and other stomach-related issues.
Ques: How do I know if it’s food poisoning or stomach virus?
Ans: Stomach viruses are only caused by viruses and affect in 24 hours. Food poisoning can be the result of viruses, bacteria or parasites. It affects almost immediately within 2-6 hrs.
Ques: When should I go to the doctor for food poisoning?
Ans: Seek urgent medical help if you have these symptoms – blood in your vomit, blurry vision, diarrhea for more than 3 days, extreme pain or cramps and fever over 101.5°F.
Ques: How can I recover from food poisoning fast?
Ans: You should drink water or electrolyte solution and avoid solid foods to recover from food poisoning quickly.
Ques: Which doctor to consult for food poisoning?
Ans: You should seek medical help from a qualified gastroenterologist in case of food poisoning.
Childhood is the time when you lay the foundation stone of your mental, emotional and physical health. Children, however, are unaware of how to make a healthy start. This responsibility, thus, falls upon the parents. As a parent or guardian, you should ensure that your kids are receiving sufficient nutrients needed for their growth. In this article, Dr. Reetadyuti Mukhopadhyay – best paediatric orthopaedic doctor in Gurgaon will explore one development aspect – How to build strong bones in kids?
Our bones start building their strength in childhood and teen years. Approximately, 95% of bone mass is built by the age of 20 years. This time is crucial for the overall internal development of a child. Though we continue to build healthy bones throughout our lives, the ability of our lives to add to this strength declines over time.
One of the important facts about muscles and bones for kids is that a better bone building ability in childhood leads to better bone strength in adulthood. It is, therefore, essential to build strong bones in kids from an early age.
Here are some expert-approved tips for strong bones in children.
Table of Contents
Children are quick learners and pick up the habits of adults they live with. The imitation capability of young kids is extraordinary and invites effort from the parents. The best tip on how to build strong bones in kids is to offer them a healthy lifestyle by implementing one.
You can inculcate bone strengthening foods in your meals to achieve a healthy living status. While making a nutritious meal plan for your kid, make sure to add plenty of the following given nutrients.
Calcium is a super-nutrient to strengthen your kids bones. The mineral responsible for building and maintaining the mass of your bones is calcium. The more calcium you eat, the stronger your bones become.
Your body’s calcium requirement fluctuate as you grow old. A child between the age group 4-8 years need nearly 1000 mg of calcium per day. While a child of 9-18 years old requires 1300 mg of calcium each day.
Dairy products such as milk, cheese, yogurt are good sources of calcium. Green leafy vegetables, soya drinks, bread, beans, lentils, almonds and fish are also rich in calcium.
How to add calcium to your kid’s diet: Children are not fans of healthy foods, popularly known as picky-eaters. It may be difficult to get your child to each calcium-rich meals. You can make the intake of calcium more interesting for your child. For instance, you can give them cookies along with a glass of milk. Children have a special liking for cheese products such as pizza and pasta. You can also choose a flavourful variant of yogurt.
It is not enough to eat calcium-rich foods alone. The consumed calcium needs to be absorbed by our bodies. Vitamin D is an important nutrient required to build healthy bones. A deficiency of Vitamin D can lead to musculoskeletal problems in children such as rickets.
The approximate unit of Vitamin D required by a kid and teenager is 600 IU per day.
The best natural source of Vitamin D is sunlight. You should make sure that your kid is getting enough sun. This tip is crucial especially in today’s times when kids tend to spend more time indoors at their tablets and television.
Bone strengthening foods rich in Vitamin D are salmon, egg yolks, mushrooms, milk, orange juice, cereal and oatmeal.
How to add Vitamin D to your kid’s diet: You can plan outdoor activities with your kids to help them get sunlight. You can replace your child’s soda or milk with orange juice now and then.
Magnesium is a vital mineral responsible for maintaining the density of your bones. A high bone density helps reduce the chances of bone fractures. Several studies have proved that magnesium also helps in the prevention of a popular musculoskeletal disorder – osteoporosis.
A young kid aged between 4-8 years should intake nearly 130 mg of magnesium per day. The daily allowance increases to 240 mg when a child reaches 9-18 years old.
This mineral also helps in the regulation of calcium and Vitamin D. You can strengthen your kids bones by including these sources of magnesium in their diet – almonds, spinach, cashews, soy milk, peanut butter, potatoes, banana, cooked brown rice, breakfast cereals and more.
How to add Magnesium to your kid’s diet: Most of the foods rich in magnesium are good substitutes of unhealthy snacks.
A regular administration of Vitamin K can increase bone density. It is useful in the metabolism of calcium and vitamin D in the bones.
A deficiency in Vitamin K can lead to an increased risk of osteoporosis. This mineral is significant for the regulating metabolism in the bone by activating proteins.
For children aged 4-8 years, 55 mg of Vitamin K per day is sufficient while 60mg/day is enough for a child in the age group of 9-18 years.
How to add Vitamin K to your kid’s diet: Try to make dishes from green leafy vegetables. Spinach, kale, broccoli, green beans, kiwi, cheese and peas are good sources of vitamin K.
Here are some interesting facts about muscles and bones for kids:
Several other parenting tips for strong bones can be used by parents besides increasing the child’s intake of bone strengthening foods.
1. Exercise more frequently: Our bones gain their strength with increased activity. Similar to muscles, your kids health bones will improve as much as he/she puts them to use. The strength of your bones increases when you put pressure on your bones by using your muscles.
A child’s potential for physical activity is better than an adult. Your kid will build strong bones if he/she does more weight-bearing activities. Running, walking, jumping and climbing are some top choices of exercise in children. You should maintain a good balance between your child’s screentime and physical activity.
2. Avoid carbonated drinks: Most carbonated drinks have some quantity of phosphoric acid. This acid is harmful to a person’s bone health as it interrupts the process of calcium absorption. You should try to replace your kid’s soda with a healthful alternative such as orange juice.
3. Teach them healthy lifestyle choices: Growing up, your child may make their own decisions and change their lifestyle habits. While a sense of liberation is important for your child’s personality development, you should ensure that he/she is not adapting wrong habits. It is especially crucial for teenagers. Smoking, alcohol consumption or leading a sedentary life are some habits that affect your bone health negatively.
By practising the above-given tips, you can help on how to build strong bones in kids. While bone health requires continuous attention, the early years of your life can help shape your future.
For more tips on how to build strong bones in kids, you can book an appointment with Dr. Reetadyuti Mukhopadhyay, leading pediatric orthopaedic doctor at the CK Birla Hospital.
Ques: At what age do children’s bones harden?
Ans: Children’s bones do not fuse until 1 or 2 years of age.
Ques: Which foods are good for bone health in kids?
Ans: Dairy products, green leafy vegetables, soya beans, tofu, nuts, bread and fish are good foods for bone health.
Ques: Which fruits are best for bone health?
Ans: Oranges, papaya, strawberries and pineapples are some great fruits for bones.
Ques: Should I give my child calcium supplements?
Ans: It is not necessary to give your child supplements. You should aim to include calcium-rich foods in their diet. Give any supplements upon your doctor’s recommendation.
Human beings have a natural tendency to be health anxious, especially with regards to some areas of our body, for instance, breasts. If you were to wake up with an abnormality in your breast size, shape, touch or appearance, you would most likely assume it to be cancer. And rightly so, considering the high prevalence of breast cancer with nearly 2 million people affected worldwide every year. However, irrespective of the rising incidence, not all breast abnormalities are cancer. Benign breast conditions (also called non-cancerous breast conditions or benign breast disease) are also commonplace and affect millions of women across different age groups.
In this article, Dr Rohan Khandelwal, a leading breast specialist in Gurgaon at the CK Birla Hospital, explains everything there is to know about benign breast conditions.
Table of Contents
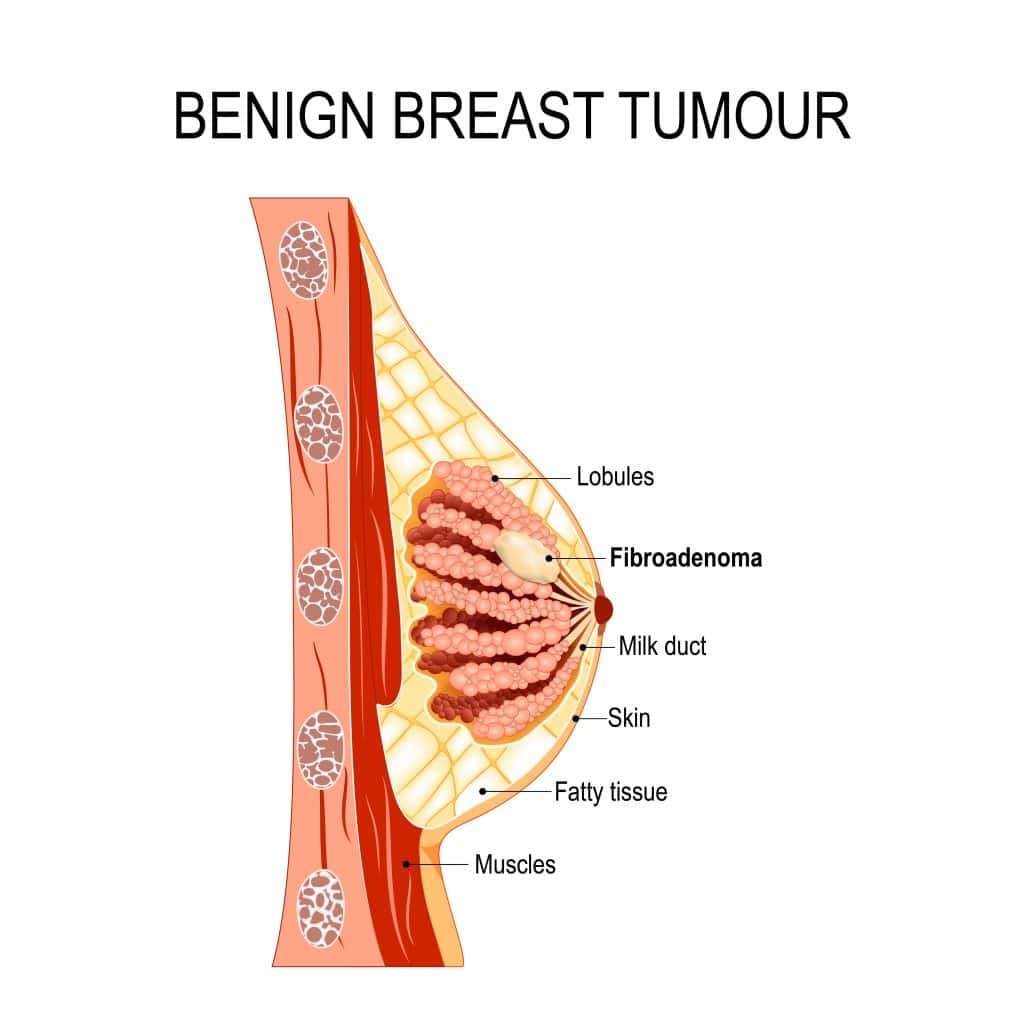
Benign, by definition, means non-malignant aka non-cancerous. Benign breast conditions (also referred to as benign breast disease) are non-cancerous tumours, growths, or structural changes that affect the breast area.
Noncancerous breast conditions indicate the presence of unusual growths that are not related to cancer cells. These growths appear in the form of breast lumps and are often misunderstood for cancerous tumours. However, about 80% of breast lumps are found to be benign upon diagnosis.
While a benign breast lump may not be directly associated with cancer, certain conditions may increase the risk of developing breast cancer in the future. Medical experts therefore classify benign breast diseases based on their cancer risk.
Therefore, benign breast lumps classification includes three categories:
Also called non-proliferative breast lumps, these are typically associated with no future risk of breast cancer.
Examples include:
The risk of cancer with such conditions is minor, but they may require regular monitoring.
Examples include:
Other conditions include juvenile papillomatosis and peripheral intraductal papillomas.
Also called “atypical ductal hyperplasia” or “atypical lobular hyperplasia”, this condition involves unusual-looking cells dividing excessively. It increases the lifetime risk of breast cancer by 3 to 5 times.
The treatment may include removal of cells around that area as well as paying closer attention to breast health.
The symptoms of a benign breast lump and breast cancer often overlap. You may feel overwhelmed and scared after discovering the initial symptoms. However, mostly, these atypical growths are diagnosed as benign. Benign breast conditions are so common that up to 50% of all women experience one such disease once during their lifetime.
There are several different types of benign breast diseases that affect every person uniquely. Only a qualified medical professional can diagnose these diseases correctly. Some common signs and symptoms of benign breast disease include:
You must consult a breast specialist even when a single symptom is seen. All of the above signs and symptoms require further testing and investigation.
Benign breast conditions can affect a person in the form of various conditions. Some common diseases include:
Since there is a wide range of benign breast diseases, there are multiple reasons why they occur. Some common reasons for the development of non cancerous breast conditions are:
Anyone can be affected by non cancerous breast conditions. However, some people are at a greater risk than others. You are more likely to have a benign breast disease, if:
It is common to mistake a benign breast lump for breast cancer. It is important that you seek urgent clinical help upon discovering any of the above-mentioned symptoms. The diagnosis of a benign breast disease starts similar to the diagnosis of breast cancer.
Your healthcare provider will order a variety of tests to eliminate the possibility of cancer and identify the type of benign disease. Some common tests include:
Other diagnostic tests may also be ordered if your doctor suspects the need for them or a suspicious lump in breast ultrasound appears.
Your treatment plan for a benign breast disease depends upon its type and severity of symptoms. Most of the benign breast diseases do not require any treatment and do not cause any painful symptoms. These conditions tend to subside on their own.
If you are wondering about breast lump when to worry, you may consult our Breast Cancer Doctor upon experiencing extreme pain or discomfort. Your doctor may offer relevant treatment, accordingly.
As mentioned above, most breast lumps shrink on their own without causing any pain or discomfort. However, you can speed up the treatment of breast lumps naturally.
Here listed are some home remedies that can help to cure breast lumps.
Please note, you should consult with your healthcare provider before applying any of these measures.
Benign breast tumor, by description, are non-cancerous. A majority of benign breast diseases do not turn malignant, that is, cancerous. However, some of them may increase your risk of developing cancer cells.
Simple and fibrosis cysts can be treated if they are causing pain or discomfort. The fluid in these cysts can be drained by inserting a thin and hollow needle in the cyst.
Benign breast conditions are highly common in women across all ages. However, these diseases are not a cause for concern.
If you detect any symptoms that may signal a problem, seek immediate health care. Frequent breast exams and timely treatment will help doctors address complications in time and suggest corrective measures.
For more information on what is benign breast disease, book an appointment with Dr Rohan Khandelwal, the best breast cancer specialist in Gurgaon at the CK Birla Hospital.
Also, watch Dr Rohan Khandelwal, Breast cancer specialist at the CK Birla Hospital sheds some more light on this condition:
Ques: Do benign breast tumours need to be removed?
Ans: If your doctor suspects an abnormality in benign breast tumour along with severe symptoms and pain, they may suggest to surgically remove it.
Ques: Can a benign breast lump turn into cancer?
Ans: No, most benign breast lumps do not turn into cancer.
Ques: What happens if you have a benign breast lump?
Ans: Benign breast lumps are non-malignant and do not usually require clinical intervention.
Ques: What does a benign breast lump feel like?
Ans: Benign breast lumps are soft and usually have smooth edges. These lumps can be moved slightly when pushed.
Ques: Is it necessary to remove benign breast lumps?
Ans: Most often, a benign lump does not need treatment. Surgery may be done if you experience pain, discomfort or other symptoms.
Ques: Are benign breast conditions & cancer common in men?
Ans: Men are at a much lower risk of breast cancer or breast conditions than their female counterparts, although they can develop similar breast conditions, too.
Those who have periods can understand that it is an agonising experience. Every month, women have to deal with aggravating pain, cramps and discomfort. The usual menstrual cycle is already painful enough. Now blend it with additional post-operative recovery and what you have is unexplainable distress. This is especially the case for the first period after laparoscopy endometriosis, a condition that affects more than 2 million women in India.
In this article, Dr Anjali Kumar, a leading gynaecologist at the CK Birla Hospital, will explore how a woman’s first period after laparoscopy surgery endometriosis treatment is like.
Table of Contents
Laparoscopy is an advanced key-hole surgery to treat endometriosis. The surgery can temporarily affect a woman’s reproductive health.
Before we look at the changes that occur during the first period after laparoscopy endometriosis, let’s understand what these terms mean.
Endometriosis is a condition in which similar tissues that line the inside of the uterus begin to grow on the outside. These tissues generally develop in the ovaries and fallopian tubes. It is a painful disorder that impacts a woman’s overall health including fertility.
Common symptoms of endometriosis include:
Laparoscopy to remove endometriosis is a surgical treatment. It is a minimally invasive method in which surgeons make small incisions in your abdomen region.
Through these incisions, they insert a thin tube attached with a tiny camera called a laparoscope. Surgeons utilise the laparoscope in viewing the insides of the uterus. They continue to remove the tissues that have grown on the outer uterus lining.
The recovery of laparoscopy is different for each woman. Due to this, the first menses after surgery and their effect also vary.
Your first menstruation will happen after 4-6 weeks of surgery. Your body is in the healing phase at this moment. So your periods will be heavily bothersome.
You can expect the following during your first period after laparoscopy endometriosis treatment:
The reason why you will feel additional discomfort is that your body is still healing internally. Laparoscopy to remove endometriosis is a surgery that directly takes place at the ovaries and fallopian tubes.
Due to the surgery, your ovaries will still be very tender. Additionally, the tissues in your ovaries and fallopian tubes would be swollen. The standard discomfort of periods overlaps with this tenderness causing excruciating pain during the first periods.
Though the first menses during recovery will be distressing, you can still cope with it. Here are some expert-approved ways to deal with the first period after laparoscopy endometriosis:
Your first period after laparoscopy to remove endometriosis will be, undoubtedly, exhausting. You can use the above-given tips to endure the pain and let this stage pass. The intensity of pain will subside gradually in the subsequent periods. You can seek instant medical support for your first period post laparoscopy surgery treatment.
You can book an appointment with Dr Anjali Kumar, the best gynecologist in Gurgaon at CK Birla Hospital, for more information or personalised guidance on endometriosis treatment.
Ques: How soon after a laparoscopy can I have my period?
Ans: You can expect your period after 4-6 week of laparoscopic surgery.
Ques: Can my first period be delayed after laparoscopy?
Ans: Yes, it is not unusual to miss or have a delayed period after laparoscopy. It can happen due to both, physical and psychological stress.
Ques: Is bleeding after laparoscopy normal?
Ans: Yes, some amount of vaginal bleeding after laparoscopy is normal. You may experience bleeding for up to a week post-surgery.
Ques: How long does it take to recover from laparoscopy?
Ans: Your recovery period depends upon your age, overall health and severity of the condition. On average, you can expect to fully recover from a laparoscopy for endometriosis in about 6 weeks.
Prostate cancer is among the top ten cancers affecting men across age groups. It is highly prevalent in India and is the 6th leading cause of death in men. Despite the figures, the rising incidence of this cancer can be controlled by practising prevention measures. Prostate cancer prevention is a conscious choice to substantially lower the risk of its spread.
In this article, Dr Shalabh Agrawal, the best urologist in Gurgaon, offers his insights on how to prevent prostate cancer.
Table of Contents
Before we help you with ways to prevent prostate cancer, let us get a general overview of what is prostate cancer all about.
Prostate cancer is the abrupt growth of cancer cells found in the prostate gland. The prostate is responsible for producing seminal fluid and promoting the reproductive health of a man.
Prostate cancer symptoms usually become visible when cancer has advanced. Some of the common symptoms include:
Prostate cancer can only be diagnosed by a verified medical expert. Most people present with the above-given symptoms and undergo a variety of tests to find that they have prostate cancer.
Any man can develop prostate cancer during his reproductive age. Some men, however, have an increased risk of getting prostate cancer (prostate cancer doctor). The common risk factors include:
Yes, prostate cancer prevention is possible and effective. Though there is no single strategy that ensures ways to prevent prostate cancer, a variety of precautionary measures can be successful.
Here are some expert-approved tips on how to prevent prostate cancer:
1. Load up on fruits and vegetables: A healthy diet filled with a range of fruits and vegetables is customary to prostate cancer prevention. Several studies have proved that the antioxidants present in these food items prevent damage to cells present in the prostate.
Red fruits such as tomatoes are rich in lycopene (an antioxidant). Lycopene has been associated with a reduced risk of prostate cancer. Other fruits and vegetables that protect against this cancer are leafy greens such as spinach, beans, peas, blueberries, grapefruit, oranges and watermelon.
2. Consider taking vitamin supplements: Vitamins and minerals are essential to our overall well-being. They are regarded as significant in prostate cancer prevention guidelines.
However, maintaining a well-balanced intake of vitamins, minerals and proteins through natural means is not always possible. Supplements help us to compensate for any nutrient demand that has not been met.
3. Exercise most days of the week: The importance of exercise for cancer prevention is crystal clear. Irrespective of your body weight, you are advised to engage in physical activity regularly.
Exercising helps promote better blood circulation, removal of toxins from the body and uplifting mood. Your immune system will be strengthened even if you exercise at least 4 days a week.
4. Maintain a healthy weight: Prostate cancer is linked with obesity – the more overweight a person becomes, the higher his chances of cancer get. One of the most natural ways to prevent prostate cancer is to maintain a healthy weight. Exercising regularly is a great path for healthy body weight. Physical activity promotes the loss of excess weight and fats.
5. Quit smoking: Tobacco consumption has a direct impact on the development of cancerous cells in the prostate gland. If you smoke cigarettes, it is your time to quit for prostate cancer prevention. If you do not smoke, we suggest that you should not start.
6. Restrict alcohol intake: An uncontrolled consumption of alcohol impacts your heart health negatively. It can additionally worsen your blood pressure levels, blood cholesterol and cause other health problems. A limit on the intake of alcohol is one of the top prostate cancer prevention guidelines. If you are already living with prostate cancer risk factors, it is advised that you restrict your alcohol consumption.
7. Take in more Vitamin D: All vitamins are essential to a healthy mind and body. However, vitamin D has additional proven effects. It is among the natural ways to prevent prostate cancer.
You should extend your exposure to the sun along with eating foods rich in vitamin D. Foods that can prevent prostate cancer and are rich in vitamin D are mushrooms, salmon and more.
8. Stay sexually active: The prostate gland has direct involvement in your sexual health. A healthy sexual life is your answer to can prostate cancer be prevented. Men who ejaculate frequently are at a safer distance from developing cancer cells.
9. Live stress-free: Stress is a leading cause of health complications in men and women. A man who lives a stressful life is often faced with problems on the sexual front.
It is necessary to monitor your way of living and perform meditation to alleviate stress levels. A sedentary lifestyle along with high-stress levels can increase the risk of prostate cancer.
10. Get early screening: Prostate cancer symptoms are not easily detectable in the early stages. Sometimes men may misinterpret these signs and symptoms of other health conditions. It should be noted that early detection of prostate cancer is the best prevention measure.
If you are living with risk factors such as obesity, old age, family history or even a sedentary lifestyle, you should consider going for regular screening for prostate cancer prevention. Your healthcare provider would offer a full range of diagnostics and imaging services to detect the presence of a cancerous cell and offer relevant prostate cancer treatment
If the cancer is found in its early stages, effective treatment can be given so that the patient feels complete relief and cancer does not occur again.
Prostate cancer prevention can be successfully done by incorporating the above-given tips in your every day.
If you wish to learn more about your risk of prostate cancer, book a consultation with Dr Shalabh Agrawal, urologist & andrologist at the CK Birla Hospital for personalised guidance.
Visit the CK Birla Hospital for more details on prostate cancer prevention guidelines and treatment.
FAQs
Ques: What are the main causes of prostate cancer?
Ans: There is no single cause of prostate cancer. Medical experts believe a change in DNA in the prostate gland leads to cancer, over time.
Ques: Can I prevent prostate problems naturally?
Ans: Yes, you can prevent prostate problems naturally by following healthy lifestyle habits that involve a well-balanced low-fat diet, regular exercise, no smoking and drinking, more vitamin D and low levels of stress.
Ques: What foods kill prostate cancer?
Ans: Foods that may help in slowing down the spread of prostate cancer include broccoli, cauliflower, cabbage, Brussels sprouts, bok choy, spinach and kale.
Ques: Does Ejaculation cause or prevent Prostate Cancer?
Ans: Medical experts have found that more ejaculation is linked to a decreased prostate cancer risk.
Most Indians are concerned and well-informed about cardiac and arthritic conditions. While, surprisingly, the incidence rate of hernia is on a rise in the Indian population. More than 1 million Indians experience this ailment annually. A hernia is a common condition that often leads to the use of surgery for treatment. It is essential to learn about what is a hernia when the prevalence is so alarming.
In this article, a leading general surgeon in Gurgaon, talks about what is hernia disease, its causes and treatment options.
Table of Contents
A hernia is a condition that leads to the formation of an abnormal localised bulge of body organs or muscle tissues. This bulge pushes through the muscles that have been holding it in its original place.
A hernia is not a fatal condition. However, it can cause major levels of discomfort. Severe cases lead to other health complications associated with hernia. A hernia can occur anywhere between your chest and your groin. Most often, it appears on the abdomen and upper thighs.
There are several different types of hernias. Most common types include:
The other uncommon forms of hernia are incisional, epigastric, spigelian and diaphragmatic hernia.
A hernia, as mentioned above, appears in the form of a bulge. Depending on the contents of hernia and its location, it may disappear when you are lying down.
The bulge can be seen and felt. It aggravates when you cough, bend or put any pressure on the specific body part. Besides a visibly abnormal bulge, pain and discomfort are the symptoms associated with this condition.
Specific types of hernia can lead to more narrowed down symptoms such as chest pain, difficulty in swallowing, heartburn and more.
One of the fundamental causes of hernia is muscle weakness. A muscular wall keeps the abdominal organs in place. When muscles responsible for holding these organs and tissues in place become weak, they lose their strength resulting in a hernia.
The chances of occurrence of hernia increase with age as muscles tend to lose their tone and become lax. There are several reasons why muscles strain and become weak leading to hernia. Sometimes a weak muscle is present since birth and causes a gradual development of a hernia problem.
The most common causes of hernia include:
The above-given factors can impact anyone at any age since muscle straining can be caused irrespective of age and gender. However, some people are more likely to be affected by this condition than others. Your risk of developing hernia problem increase if:
A hernia problem is easily diagnosed with the help of a physical exam. Your healthcare provider (hernia doctor)will simply need to feel and analyse the bulge. Your doctor will evaluate your condition based on the information you provide regarding the severity of your symptoms.
Your doctor will ask you the first time you noticed a hernia, the kind of pain and discomfort it had been causing you, your lifestyle habits, your family history of the disease and your personal medical history.
If your doctor may suspect the need for additional screening tests to evaluate the location and contents of hernia properly. The additional tests include abdominal ultrasounds, CT scans, MRI, endoscopy and more.
Sometimes hernia problem can subside on its own. However, most of the times, it requires surgical intervention. If you have mild symptoms, your healthcare provider may suggest watchful waiting as a treatment protocol. Your condition will be monitored consistently and you will offer pain relief support.
If your symptoms are severe, your hernia treatment options only include surgical repair. Surgery for hernia can permanently fix your problem and give you instant relief from pain and discomfort.
Both hernia treatment options are highly effective and safe. However, small risks and complications such as infection, low-grade fever are associated with hernia surgery.
The laparoscopic surgery offers more benefits to the patients as compared to open surgery. It requires less hospital stay, bleeding, scarring and a decreased chance of infection.
An active and healthy lifestyle is the key to hernia prevention. You should practice the following tips and tricks to keep hernia at bay:
Prevention is only possible when most people grasp the concept of what is a hernia. Even if you have a non-symptomatic hernia, you should get it inspected by a healthcare provider to avoid any medical complications.
Ques: How serious is a Hernia problem?
An untreated hernia can cause various life-threatening complications. A hernia can get bigger and more painful.
Ques: Is a hernia painful?
Pain is a common symptom of hernia. However, whether the hernia is painful or not depends upon the location and size of the hernia.
Ques: What type of Hernia is most severe?
According to research, umbilical hernia is considered most severe among all types.
Ques: Do Hernias always require surgery?
Most hernia requires surgical intervention for permanent relief. Surgery is indicated only when the hernia is usually getting bigger with severe symptoms.
Often pain in the shoulder is inappropriately given a blanket diagnosis of ‘frozen shoulder’. The first course of action by most people is to undergo physiotherapy. However, it is not enough to have untargeted physical therapy without proper diagnosis. More than 50% of older adults with diabetes are affected with frozen shoulder. It is, thus, important to understand the basics of this ailment. In this article, Dr Reetadyuti, the best shoulder specialist in Gurgaon, offers a complete guide of what is frozen shoulder and how to diagnose frozen shoulder.
Table of Contents
Frozen shoulder is a common musculoskeletal disorder that affects the shoulder joint. It is medically referred to as adhesive capsulitis.
This condition characterised by shoulder stiffness, pain and a restricted range of motion.
Primarily, the symptoms of a frozen shoulder include a dull pain and shoulder stiffness. You may also experience a similar pain spreading to your upper arm. In this condition, the sensation of discomfort tends to worsen in night.
A frozen shoulder progresses gradually in three stages. Each stage has a distinguished set of symptoms to look out for:
The anatomy of your shoulder consists of three bones. These bones are structured in a way that forms a ball and socket joint protected by a capsule of connective tissues. Over time, the connective tissues in the shoulder joint can become thicker, tighter, and inflamed. This stiffness limits the mobility of your shoulder and causes severe pain.
Frozen shoulder can affect any person irrespective of their age and gender. However, some population groups are more likely to be affected by this condition. The common risk factors for developing frozen shoulder are:
Your healthcare provider will discuss your medical history with you. He/she will ask you about the symptoms, the first time you noticed pain and stiffness and the effect of symptoms in your routine.
A general physical exam and frozen shoulder test are enough to diagnose frozen shoulder. There are three essential elements of a frozen shoulder test.
Your shoulder specialist may also order some imaging tests such as X-rays and MRI scans to rule out the possibility of other musculoskeletal conditions such as arthritis or rotator cuff tear.
The fundamental step on how to cure frozen shoulder quickly is pain management. As the stage progresses, your healthcare provider may indicate other treatment modalities to get rid of frozen shoulder.
Hot and cold compress: Based on your diagnosis and severity of symptoms, your healthcare provider will suggest either a hot or a cold compress. Heat and cold compresses help reduce the pain and stiffness in the joint.
Medicines: Your doctor will prescribe relevant pain relief medications for your condition. The alleviation of pain is the foremost step towards frozen shoulder treatment.
Physical therapy: As your pain and swelling subside, your doctor will progress the treatment by indicating physiotherapy. A trained physical therapist will perform stretching exercises to improve your range of motion.
Surgical procedures: Mostly a frozen shoulder gets better with the use of medicines and physiotherapy within a few months. Nevertheless, there are rare incidents that require surgical intervention. Your healthcare provider may indicate joint distension, shoulder manipulation and other arthroscopic procedures to treat persistent frozen shoulder.
Though frozen shoulder causes and cure are often overlooked, it is possible to prevent the incidence of frozen shoulder, especially when you are recovering from a shoulder injury. Physical therapy by a verified therapist is a great preventive measure. If you have suffered from a shoulder injury or begun experiencing pain, you should avail physiotherapy to stop the condition from progressing further.
Some exercises can also be done routinely at home. Your healthcare provider can help formulate an effective exercise regime for you to practise at home.
If it is not treated properly, a frozen shoulder can cause long-lasting pain and immobility. A timely and proper diagnosis is crucial to care for a frozen shoulder. Your shoulder specialist will guide you towards a healthy lifestyle that includes activities suitable for your shoulder joints.
Book an appointment with Dr Reetadyuti, the best shoulder specialist in Gurgaon at the CK Birla Hospital, to learn more about the shoulder and joint conditions.
Ques: What is frozen shoulder pain like?
Frozen shoulder pain is like a dull and achy pain in the shoulder that may worsen during the night.
Ques: Is it OK to massage a frozen shoulder?
Yes, you can massage and stretch a frozen shoulder to relieve tension and tightness.
Ques: Why does a frozen shoulder hurt more at night?
It is because, during the night, when you lay down, the inflamed area of your shoulder becomes compressed and causes increased stiffness and pain.
Ques: Is surgery an option for frozen shoulder?
Yes, surgical repair of a frozen shoulder is an option. However, most frozen shoulders are treated non-surgically.
Three factors are interpreted for increased incidences of ankle injuries – slippery surfaces, sports and high heels. It is, however, possible to hurt your ankle at other places and situations. Even a casual walk around the neighbourhood can make you trip and fall, sometimes leading to an ankle fracture. According to a study by the Indian Journal of Medical Research, more than 69% of people in Delhi between the age group 35-68 suffer from a high risk of bone fractures. The incidence of ankle fracture alone is 187 fractures per 100,000 in a year.
In this article, , foot and ankle specialist at the CK Birla Hospital will explore everything you need to know about a fractured ankle and the possible causes leading to such high incidence.
Table of Contents
Ankle fracture happens when a bone in the ankle joint gets broken. This injury is also referred to as a broken ankle. A fractured ankle can range from a tiny crack in the bone to a complete dissociation where your bone peaks out of the skin.
An ankle joint is structured with three bones – tibia which forms the medial and posterior malleolus; fibula which forms the lateral malleolus and talus. A fracture is characterised based on the bone that has been affected.
There are various types of ankle fractures. The fractures which involve only one bone can be medial or lateral malleolus fractures. The fractures that involve two or three malleoli are called bimalleolar and trimalleolar fractures respectively. Apart from the broken bones, the ankle fractures may be associated with injury to a ligament called syndesmosis which binds the lower end of tibia and fibula together.
Ankle fractures are caused by abnormal twisting, rolling, tripping or trauma of the ankle. Some of the common causes for a fractured ankle include:
While everyone can suffer from a fractured ankle, some people are more likely to experience this injury. If you play high-impact sports such as basketball, gymnastics, football and more, your chances of having a broken ankle increase. Walking on uneven surfaces can result in more trips and falls. Decreased bone density or conditions such as osteoporosis can also raise your possibility of ankle fractures.
Your pain-bearing capacity can sometimes misinterpret a fracture. You should look out for the following fractured ankle symptoms:
The location and extent of swelling in a broken ankle will depend on the type and location of the fracture.
As mentioned above, the pain management capacity of individuals can, sometimes, cause misunderstanding about an injury. So how do I know if I have broken my ankle?
An ankle sprain is an injury of tendons and ligaments. When the ankle ligaments tear or stretch, they can cause pain and swelling. Pain and swelling are also fractured ankle symptoms.
Your healthcare provider will be able to diagnose your injury properly. You should note that the severity of symptoms is immense when an ankle is broken while an ankle sprain can be easily managed.
Also, watch the video as Dr Anuj Chawla – Foot & Ankle Specialist at the CK Birla Hospital, sheds some light on ankle fractures and the steps you can take to minimise its impact.
Your healthcare provider will first assess your injury before providing ankle fracture treatment. He/she will physically evaluate the mobility of your foot by moving it in different positions. Your doctor will ask you about your symptoms.
Your doctor will order a few imaging tests to precisely diagnose the condition. The following tests are indicated in case of a fractured ankle:
Ankle fracture treatment depends upon the location of the fracture and severity of symptoms. Conservative treatment is offered in mild cases. If your ankle is stable, your hairline ankle fracture can recover by non-surgical means. While treating the ankle fracture non-operatively, immobilisation in a rigid cast or boot for 6-8 weeks is undertaken.
Most of the times, ankle fracture surgery is performed to treat the joint. Surgery is performed to reduce the displaced fragments to their original place and then fixing it with plates and screws. This method is also called as Open Reduction and Internal Fixation.
Physical therapy is important for recovery from a fractured ankle. You should consult a verified physical therapist for your treatment. Physical therapy is critical for restoring and improving the strength of your bones.
Fractured ankle recovery time depends upon the severity of your condition. If you have had a procedure to correct a broken ankle, you can expect recovery within 8-12 weeks. You are expected to follow your doctor’s guidelines and provide complete rest to experience a quick recovery.
Based on your injury, your doctor will offer you relevant broken ankle recovery tips. Practice the following tips during recovery:
Since the ankle fracture affects your joint, it is not advisable to put weight on your broken ankle for the first few weeks. Your ability to walk depends upon the type and seriousness of the fracture you have encountered. If your fracture is mild and hairline, your doctor may allow you early weight bearing and walking on your ankle.
However, a serious broken ankle will take time in recovery and delay walking. Walking on a broken ankle too soon may result in unbearable pain or discomfort from the slightest of movement.
Your doctor will assess and supervise your recovery. He/she will suggest when you can walk after a broken ankle.
Your physiotherapist will provide support in this process. He will help improve your movement of ankle and bone strength. You can also choose to start walking with the help of walker, cane or crutches.
Ankle fracture is not an uncommon condition, but it requires urgent medical intervention. An untreated fractured ankle can cause several health complications such as arthritis, persistent pain, ligament injury, nerve damage and more.
To learn more about musculoskeletal health, consult Dr Anuj Chawla at the CK Birla Hospital.
Ques: Can you walk on an ankle fracture?
Ans: The ability to walk after an ankle fracture depends upon the severity of fracture. If the fracture is minor, you may be able to walk soon. If it is serious, you will be advised to rest until the injury is healed.
Ques: How long does it take to heal a fractured ankle?
Ans: On average, it takes nearly 8-12 weeks for ankle fractures to heal completely. The recovery period may vary based on your overall health and age.
Ques: Do you need a cast for a fractured ankle?
Ans: Yes, your ankle will be placed in a cast for nearly 4-8 weeks to promote healing.
Ques: What happens if a fracture is left untreated?
Ans: An untreated fracture can lead to bone deformity, muscle and ligament damage, arthritis and persistent pain.