Blood in stool (rectal bleeding or haematochezia) can refer to any blood that passes from the anus, although blood in the stool is usually assumed to refer to bleeding from the lower colon or rectum. However, not all bleeding passing out from the body comes from the rectum. The blood or blood clot can come from anywhere in the gut. The correct term used in medicine is gastrointestinal tract bleeding.
Normally, blood in stool is a symptom rather than a condition by itself. Thus, bleeding in stools could be an indication of an underlying condition or problem and must be taken seriously.
Table of Contents
Typically, blood in stools indicates bleeding in the digestive tract. However, when you delve deeper into what does blood in stool indicate, the following reasons for blood in stools come to light:
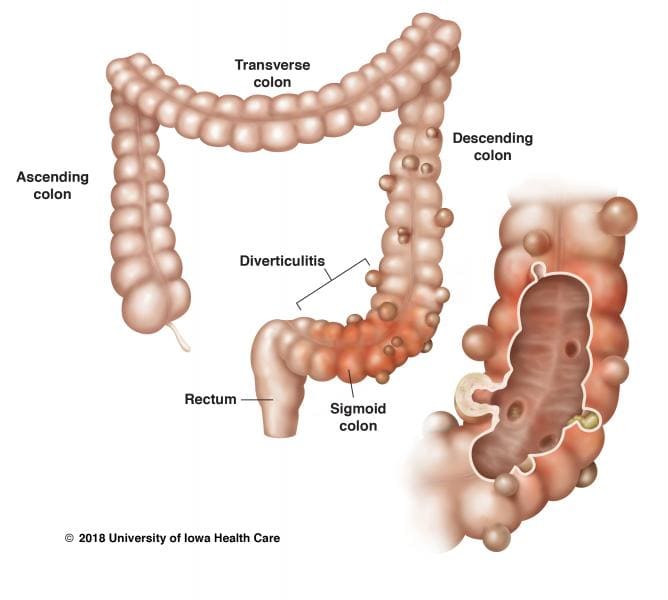
Although the prevalence of diverticulitis in India is 1-3%, it could be the reason behind abdominal pain and bleeding. Diverticula are small pouches that form on the colon wall. The formation and excessive growth of the diverticula up to several centimetres cause diverticulosis. The infection of these overgrown diverticula causes diverticulitis.
Ischemic colitis often affects the elderly and is caused by inadequate blood flow to the colon. In addition to blood in stools, ischemic colitis also exhibits symptoms of diarrhoea, abdominal pain, and vomiting. Thus, if you experience no constipation but blood in stools, you may have ischemic colitis.
If you experience blood in stool but no pain, it is possible that the pigments in foods consumed have resulted in red-coloured stools, which may be mistaken for blood.
IBD is an autoimmune disease that causes inflammation of the bowels. Crohn’s disease and ulcerative colitis are the most prevalent forms of IBD.
Blood in stools could also be an indication of colorectal cancer. Polyps, which are benign tumours that eventually grow and become cancerous, can also cause bleeding in the stools.
Today, we will discuss at-length the commonest blood in stool causes, namely, piles and fissures.
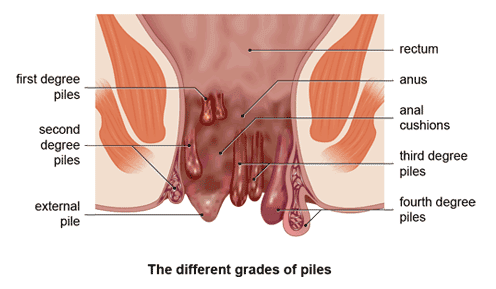
Piles, also known as haemorrhoids, are characterised by inflamed blood vessels, muscles, support tissue, and elastic fibres in the anus and rectum.
These could be internal or external and are categorised from Grade I to IV.
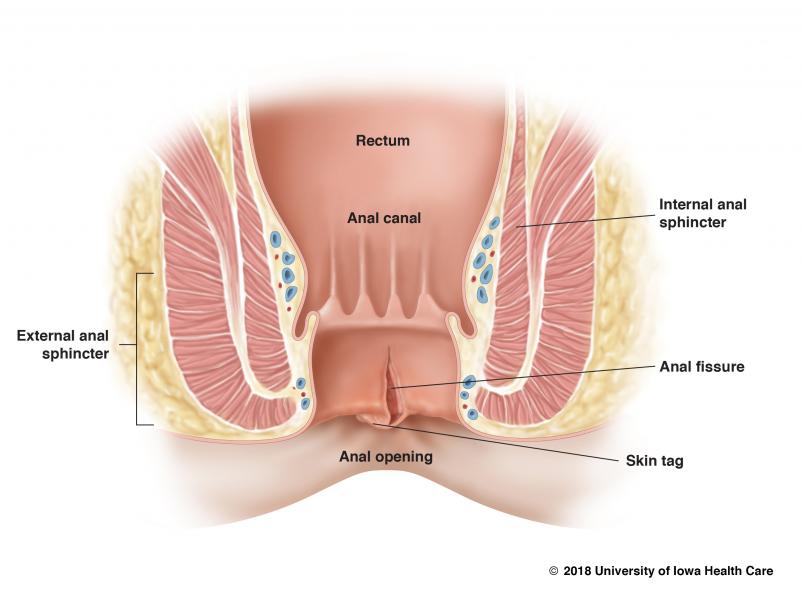
Anal fissures are a tear in the anal lining. The cut in the skin caused by hard stools that come with blood flow and severe pain after every bowel movement.
It may take the body about 4-6 weeks to recover from an anal fissure. On the other hand, severe cases may result in the exposure of the muscle tissues present underneath.
The risk of having blood in your stool could increase if you have:
Unknown bleeding inside the body is always a reason for you to get a diagnosis from your doctor. Seek medical help if the bloody stool persists for more than two days or if you are experiencing diarrhoea that is not becoming better.
You should receive medical treatment at the earliest if you develop additional symptoms, including:
To confirm the diagnosis, your doctor may order several diagnostic tests, including:
The initial treatment for blood in the stool is to stop the bleeding. Once the bleeding has stopped, your doctor will suggest a plan to treat the cause of the bleeding.
Depending on the cause, your doctor may recommend:
If you spot blood in your stool, it need not always be a cause of concern. But if the bleeding persists for more than two days, consulting a gastroenterologist is a must. If you are concerned about bleeding in your stool or if you have any other stomach problems that you need help with, you can book an appointment with our consultants, or you can reach us at +91 124 4882200
Consult a doctor for blood in stools now!