Filter :
Abdominal pain in children is a common complaint. It can be caused by various conditions, including constipation, gas, indigestion, abdominal muscle strain, and infections.
Sometimes, the cause is not apparent even after tests are done. In these cases, it’s essential to find out what’s causing your child’s symptoms so you can help your child feel better as quickly as possible.
Children can experience pain in the right lower abdomen to the upper abdomen and sometimes even as far as the chest (although this is rare). This type of pain can be:
Table of Contents
Common symptoms of children’s abdominal pain include:
The best way to help your child explain their pain symptoms is to discuss them. It’s vital for you and your child to understand the problem so you can discuss it with your doctor, who can devise a treatment plan.
Discussing pain with children can be challenging because they often don’t know how to describe their feelings. The following tips may help:
If your child is younger than six months old, contact a doctor right away if their belly looks swollen or distended (like a balloon being blown up). This could be from an intestinal blockage or other serious problem.
If your child is six months or older, call the doctor if:
These symptoms may be signs of appendicitis.
As a rule of thumb, you should see your doctor if your child:
A doctor diagnoses abdominal pain in children and babies after a thorough physical examination, history and investigations.
Diagnosing abdominal pain starts with a medical history and physical examination. Your doctor will inquire about the timing and location of the pain and how long it lasts.
They’ll ask questions about recent nausea, vomiting or diarrhoea your child has experienced. Your doctor will also examine your child’s abdomen to look for signs indicating an underlying problem.
Paediatricians use special techniques to pinpoint the cause of stomach pain in children. Some of these techniques include:
The most common cause of abdominal pain in children is a viral infection. The pain can be severe and usually go away in a few days.
If your child has pain in the lower abdomen, here’s what to do:
Abdominal pain is a common problem among children, and multiple potential causes of acute, recurrent, or chronic abdominal pain exist.
If your child complains of abdominal pain unrelated to food poisoning or constipation, consult a pediatrician at the CK Birla Hospital, or book an appointment with Dr Anukalp Prakash to learn more about treatment options.
It’s essential to understand the different types of lower abdominal pain in children and what they mean so that you can determine if your child needs urgent medical care.
Ask them the following questions:
Tummy aches are common in children. It’s essential to watch for signs (like a fever) that could signal a more serious problem and get help if needed.
If you don’t know when the fever started or how high it got (or if it came on suddenly), call your doctor immediately since it might be an infection that needs treatment.
Table of Contents
Diabetes insipidus is a disorder in which the body produces too much urine and is not able to retain water.
People with this condition pass urine frequently and drink large amounts of water. They tend to feel thirsty all the time since their body finds it difficult to retain water.
Diabetes insipidus can be a chronic condition or a temporary one. It may be mild or severe, depending on what is causing it. It is usually caused by an issue with the antidiuretic hormone (ADH).
Symptoms of diabetes insipidus may be mild or severe, depending on your specific condition. The main symptoms are as follows:
Other diabetes insipidus symptoms you may experience include:
Diabetes insipidus is caused by issues with your body’s ability to retain water and regulate fluid levels. Your kidneys filter out excess water and fluid from your body and remove waste products.
This condition is usually caused by problems with the ADH hormone (also called vasopressin), which helps your kidneys balance the fluid levels in your body. It can also be caused by issues with the part of your brain that stimulates thirst. The diabetes insipidus causes differ based on different types.
Sometimes, there is no certain cause of diabetes insipidus. In certain rare cases, the disorder may be caused by an autoimmune condition or response that makes the immune system attack the cells that make vasopressin.
There are 4 different types of diabetes insipidus. They are as follows:
This is caused by damage to the brain, which affects the release and regulation of ADH in the body.
This is caused by a structural defect in the kidneys that affects their response to ADH.
This type of diabetes insipidus is rare and occurs during pregnancy. It is caused when an enzyme released by the placenta starts to destroy ADH in the mother.
This is caused by damage to the part of the hypothalamus (in the brain) that regulates thirst.
If left untreated, diabetes insipidus can lead to more serious complications. These include:
Diabetes insipidus is diagnosed through different tests and methods.
The main tests for diabetes insipidus diagnosis include the following:
You will be asked not to drink any fluids for several hours. This stimulates your body to produce ADH. The doctor will then measure your ADH levels to determine if your body is producing enough ADH. The doctor may also measure other factors such as urine output.
Your doctor may suggest a blood test to check your ADH levels. Your blood and urine may also be tested for glucose (blood sugar), calcium, and potassium.
An MRI scan is used to check for abnormalities in the pituitary gland and hypothalamus in the brain.
If factors in your family suggest a genetic cause, your doctor may recommend genetic screening.
Diabetes insipidus treatment differs based on the type. The treatments are as follows:
If you have mild diabetes insipidus, increasing your water intake may be sufficient, and medication may not be required.
If the condition is caused by an abnormality in the pituitary gland or hypothalamus, your doctor will treat the lack of ADH. It is usually treated with desmopressin, a hormone that works similarly to ADH. It is taken as an injection, a pill, or a nasal spray.
It is usually treated with diuretics, which reduce the urine produced by your kidneys. It may also be supplemented with medication to reduce your urine volume.
There is no specific treatment for dipsogenic diabetes insipidus. However, if it is caused by an underlying issue such as a brain-related condition, treatment can target the cause.
Treatment for people with gestational diabetes insipidus is often administered in the form of the hormone desmopressin.
Certain factors can contribute to your risk of developing diabetes insipidus. These factors are as follows:
Diabetes insipidus can be uncomfortable and difficult to live with. If the condition is not addressed, it may lead to severe dehydration and other complications.
If you are facing any symptoms such as excessive thirst and frequent passing of urine, it is best to get it checked by a medical specialist.
To avail of the best diagnosis and treatment for diabetes insipidus, visit the CK Birla Hospital or book an appointment with Dr. Abhay Ahluwalia
The 4 types of diabetes insipidus are as follows:
1) Central diabetes insipidus (problems with ADH in the body)
2) Nephrogenic diabetes insipidus (structural defect in the kidneys)
3) Gestational diabetes insipidus (occurs during pregnancy)
4) Dipsogenic diabetes insipidus (problem with thirst function)
Diabetes insipidus and diabetes (diabetes mellitus or Type 1 or Type 2 diabetes) are two distinct conditions.
Diabetes mellitus happens because your body is not producing enough insulin or is not able to use it well. Diabetes insipidus occurs because your body is not producing enough antidiuretic hormone (ADH) or your kidneys are not able to use it properly.
You can be diagnosed with diabetes insipidus at any point in your life.
Central diabetes insipidus can often be diagnosed in infants as it is related to a brain condition that is present, affecting the hypothalamus and pituitary gland.
Nephrogenic diabetes insipidus may also be diagnosed in infancy or early in life as it is often caused by a genetic condition.
Gestational diabetes insipidus is diagnosed when you are pregnant.
Diabetes insipidus may be a chronic condition or a temporary one. It can be treated if it is caused by a treatable underlying condition.
However, if it is not a treatable condition (which is often the case with dipsogenic diabetes insipidus), then it may be a chronic condition.
Going through a miscarriage can be emotionally, mentally, and physically draining for an expecting mother, especially as it is completely out of your control. While there are some safety measures and precautions you can take to ensure a full-term pregnancy, miscarriages are often sudden.
You Can Also Read: A Guide to Increasing Baby Weight When 9 Months Pregnant
Table of Contents
Miscarriage refers to the loss of the embryo or foetus before the 20th week of pregnancy. A normal pregnancy lasts about 40 weeks or 9 months. The total period of the pregnancy is divided into three trimesters.
The first trimester is from week 1 to 12, the second trimester is from week 13 to 28, whereas the last and the third trimester goes from week 29 to 40. Miscarriages can happen during any of the three trimesters, but most occur before the 12th week of pregnancy, i.e., the first trimester. Hence, the first trimester is often very crucial, requiring regular monitoring.
Going through a miscarriage does not necessarily signify something wrong with you. Reasons for miscarriage can range from chromosomal abnormalities, hormonal imbalances, uterine abnormalities, malnutrition, accidental trauma, etc.
Miscarriages are very common; almost 1 in 8 pregnancies end with a miscarriage. Often, mothers might miscarry even before they become aware of their pregnancy. Additionally, a lot of women struggle with repeated miscarriages. Depending on the medical situation of each woman, miscarriages are broadly divided into 5 major types:
In a missed miscarriage, there are no typical signs and symptoms. However, when an ultrasound is performed, it shows an embryo without a heartbeat or an empty embryo sac.
If a woman undergoes three recurrent pregnancy losses, she is diagnosed with the risk of a recurrent miscarriage.
In complete miscarriage, there is a total loss of pregnancy with vaginal bleeding. All the foetal tissue passes out of the vaginal opening.
As the term ‘threatened’ suggests, in a threatened miscarriage, there is fear of miscarrying during the entire pregnancy due to risk factors like abnormal vaginal bleeding and abdominal pains. Around 50% of threatened miscarriages end in normal pregnancies, whereas the other 50% end in pregnancy loss.
An inevitable miscarriage occurs when there is excessive bleeding and the cervix begins to open. The embryo’s chances of survival in such a case are zero.
It is a misconception that routine activities like exercising, sexual activities, dancing, etc., are reasons for miscarriage. An expecting mother can continue all her regular activities in moderation while following safety precautions.
If you have underlying medical conditions, your doctor will advise you accordingly. The actual causes of miscarriage are several:
Oftentimes, expecting mothers might not even be aware that they are miscarrying. Having said that, some miscarriage symptoms and signs to watch out for are as follows:
Some risk factors for miscarriage are:
If a woman undergoes a complete miscarriage, the foetal tissue emerges via the vaginal opening. In such a case, no further treatment is required. However, in other cases, if a miscarriage has occurred and the tissues have not exited the body, the doctor will have to remove them.
Often doctors opt for the dilation and curettage procedure in which the cervix is dilated, and all the remaining tissues are removed using a surgical tool. Nowadays, medication is also available to remove the remaining tissue from the uterus. If a miscarriage occurs in the later stages of the pregnancy, when the foetus has been completely formed, the doctor will induce labour and deliver a stillborn baby.
In cases like recurrent miscarriages, the doctor will closely monitor your pregnancy. They might routinely schedule tests like a pelvic ultrasound, hysteroscopy, hysterosalpingogram, etc., to make sure the pregnancy is progressing well.
A miscarriage does not imply that you cannot get pregnant again. You will have to be cautious and follow more precautions and safety measures. 85% of women go on to have normal pregnancies after miscarrying for the first time.
In case of recurrent miscarriages, with proper advice from the doctor, it is possible to become pregnant again. You can schedule tests like chromosome tests, hormone tests, ultrasound, and blood tests to understand all the risk factors closely and proceed accordingly.

It can take a few weeks for your body to recover from the stress of miscarrying. After a miscarriage, you might also need time to heal yourself emotionally. You might experience strong feelings of loss and grief.
After a harrowing miscarriage experience, many couples find it difficult to plan their next pregnancy. Health conditions also make this difficult. Keep in mind that there is no rush to plan your next pregnancy; you can take your time to deal with your emotions.
Are you struggling with a tumultuous miscarriage and wish to find a professional and experienced health practitioner to help? Visit the CK Birla Hospital near you or book an appointment with Dr. Aruna Kalra who will help you learn about your condition and provide you with the best treatment options available.
Q1. How long does a miscarriage last?
A miscarriage can last from a few hours to a few weeks. Symptoms like abdominal pain and vaginal bleeding are normal during pregnancy, but the moment you notice something abnormal, you are advised to visit a doctor as soon as possible.
Q2. What happens first during a miscarriage?
If a woman is miscarrying, she might notice some initial symptoms like spotting, vaginal discharge, and bleeding. The cramps might also get worse with time. Symptoms differ for each woman, but the common symptoms are usually cramping and bleeding.
Q3. How do miscarriages start?
The start of the miscarriage varies for each woman. Normally miscarriages start with abdominal cramping and vaginal bleeding. With time, the symptoms worsen. It is thus advisable to visit a doctor as soon as possible.
Q4. What should you not do after a miscarriage?
Refraining from putting anything in your vaginal opening for the next few weeks after miscarriage. Avoid using period products like tampons and menstrual cups. Give yourself time to heal emotionally and mentally.
Personal hygiene is a crucial part of staying healthy. Excess humidity, a warm climate, and lack of personal hygiene are enhancing factors of UTIs (urinary tract infections), which include Chlamydia trachomatis.
However, unlike yeast overgrowth or fungal infections, the transmission of chlamydia happens through sexual contact.
Chlamydia is a silent spreader because there are no visible symptoms during its incubation period (lasting between a few weeks to six months). Besides, individuals having active and unprotected sex life are most vulnerable to contracting it.
Table of Contents
Named after its causative agent, Chlamydia trachomatis, chlamydia is a bacterial infection that affects the reproductive tract in both genders.
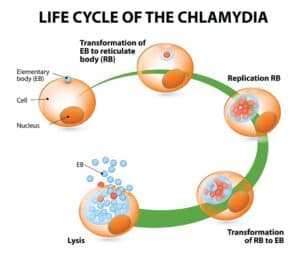
Chlamydia is the most prevalent STI, spreading rapidly often without the knowledge of the carrier, given the dormant character of the bacterium.
This condition can stay undetected until intense physical discomfort (pain during intimacy, difficulty in passing urine, or pelvic pain) post-incubation. Besides, chlamydia isn’t incurable like HIV. Seeking prompt treatment can cure this bacteria-borne STI.
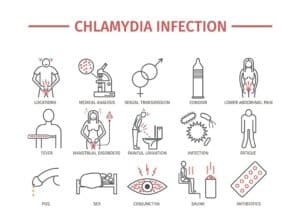
Chlamydia infection spreads through sexual contact (both oral and penetrative). It can also infect a healthy individual using sex toys or indulging in self-pleasure with a silent carrier. Prevalent pathways include:
We understand the stigma associated with STI patients, especially since most are incurable. While chlamydia is curable, some things that don’t lead to the spreading of the bacteria are as follows:
Chlamydia affects irrespective of gender, making both men and women silent carriers.
Symptoms displayed are different for both genders. It’s difficult to self-diagnose because they resemble PID (pelvic inflammatory disease) and cervical issues (cervicitis).
Here’s what chlamydia in men and women looks like:
Chlamydia is a UTI (urinary tract infection). It can affect the urogenital tract, secreting discharge from the penis. The following symptoms suggest chlamydia in men:
Besides, most men often report being asymptomatic for a long time. If you are having oral sex with a suspected Chlamydia trachomatis patient, you might develop throat issues rather than contamination around the urinogenital tract.
Chlamydia infection in women often stays hidden, devoid of symptoms immediately after contracting this STI. Prevalent symptoms show similarities with ovarian problems like PCOS and ovarian torsion, worsening the issue if the patient attempts to self-diagnose.
Here’s what to look for in chlamydia among women:
Women are prone to be silent carriers of chlamydia infection. It can also infect the rectum (anal penetration) and throat (oral sex), making it deadly enough to affect various parts of your body at once.
Contracting chlamydia requires:
Chlamydia trachomatis can only spread through sexual contact between a healthy person and a potential silent carrier. People at risk of contracting it include:
Here are the risks associated with having chlamydia in men:
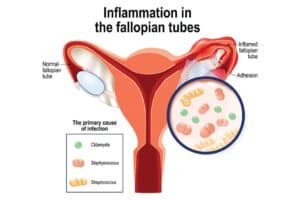
While chlamydia in women has serious side effects for both the mother and her unborn baby, complications include:
Chlamydia is a curable illness. Although chlamydia prevention is the best choice, antibiotics are the preferred treatment (since chlamydia trachomatis is a bacterium).
Your physician may prescribe you the following antibiotics:
Besides treatment, preventive behavior is the best course for chlamydia prevention. It includes:
Before making an appointment with your physician, know the chlamydia symptoms well or look for its gender-based side effects. You should make an immediate appointment if you are:
It’s crucial to maintain sexual distinction to prevent the spread of chlamydia infection. Never hesitate to reach out to your physician if you show suspected symptoms similar to chlamydia.
Not sure where to discuss your chlamydia symptoms with privacy? Visit the CK Birla Hospital near you or book an appointment with Dr. Astha Dayal to learn more about chlamydia treatment.
Q1. Is chlamydia a serious STD?
Chlamydia is a curable STD, making it not a severe condition, unlike HIV. However, if left untreated, it worsens to affect both the testis (reducing fertility) and fallopian tubes (risking ectopic pregnancy).
Q2. How do I know if I have chlamydia?/How to know if you have chlamydia?
Chlamydia symptoms, like a burning sensation during urination or smelly discharge from the urethra/vagina, show suspected signs of underlying chlamydia infection.
Q3. How long does chlamydia last?
Chlamydia infection can last for years when neglected and left untreated. Being a bacterial infection, it will keep on worsening the afflicted area unless treated with antibiotic therapy.
Q4. Does chlamydia have a smell?/Do chlamydia symptoms have a characteristic smell?
The most characteristic chlamydia symptoms include smelly and sticky discharge from the urethra and vagina. Besides, patients experience pelvic inflammation (women) and intense pain in the testis (men).
Q5. Can chlamydia go away without treatment?/Can chlamydia go away naturally?
Chlamydia is a bacterial infection contracted sexually, meaning it’s unlikely to go away naturally unless reduced through a preventive lifestyle or cured through antibiotic therapy.
Table of Contents
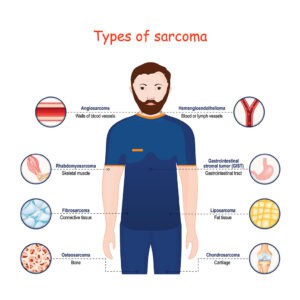
Sarcoma is a cancer of the body’s connective tissues, which include fat, muscle, nerves, tendons, and ligaments.
Sarcomas are extracted into different subgroups based on the type of cells within them. There are more than 20 types of sarcoma based on cell lineage. One common feature of sarcomas is that they often contain areas of dead tissue (called tumour necrosis).
Sarcoma can show symptoms at any age, but most cases are diagnosed in people aged 20 to 40. Sarcomas often occur in the arms or legs but can also develop in other body parts, including the pelvis and abdomen.
There are two main types of sarcomas:
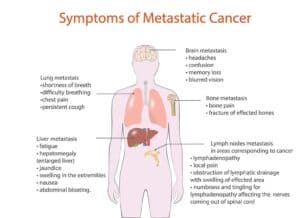
Sarcoma cancer develops slowly. It often doesn’t cause symptoms until it has spread to nearby tissues or organs.
Sarcomas do have a few early symptoms, though, which may include:
A sarcoma can be caused by:

A sarcoma is not a single disease but a term that describes any type of cancer that develops in the body’s soft tissue. Soft tissue refers to the muscles, tendons, fat and blood vessels. Risk factors for sarcoma include the following:
There are many treatment options for sarcoma, including surgery, chemotherapy and radiation therapy. Treatment depends on the type of sarcoma you have, its size, location and grade (how much it has grown).

If the cancer has spread beyond the area of your original tumour, other treatments may be needed:
Due to the diverse and often subtle nature of sarcoma symptoms, many patients are misdiagnosed and suffer until they are finally correctly diagnosed by a doctor. This is why early, accurate diagnosis is imperative.

The earlier the sarcoma is discovered, the easier it is to treat and cure. To learn more about the best treatment options for sarcoma, visit the CK Birla Hospital or book an appointment with Dr. Vinay Samuel Gaikwad.
1) Is sarcoma a serious cancer?
Yes, sarcoma is a serious cancer. It can be difficult to treat because it spreads quickly and grows in bones, fat, muscle and other organs. It also has a high rate of recurrence and metastasis (spread).
2) What type of cancer is sarcoma?
Sarcoma is a cancer that develops in the soft tissue. It can affect any area of the body, including muscles, tendons, fat, nerves and blood vessels.
3) How do you get sarcoma cancer?
The cause of sarcoma cancer is not known. It can be the outcome of a combination of factors, including:
4) What is the life expectancy with sarcoma?
The life expectancy with sarcoma depends on the type of sarcoma, where it has occurred, and whether it has spread to other parts of the body.
For example, patients with osteosarcoma have a survival rate of 70% five years after diagnosis, and those with Ewing’s sarcoma have a 5-year survival rate of 40%.
Genital herpes is a commonly found sexually transmitted disease. As many as 1 in 5 people have it, although most don’t know because it often doesn’t cause any noticeable symptoms. Whether or not to get tested, disclose your status, and use protection with new partners are all personal decisions that only you can make after learning everything about genital herpes below.
If you think you might have contracted it or are concerned about a loved one who may have it, it’s important to familiarize yourself with this disease, including its symptoms, treatment options, and ways to protect yourself from contracting it in the future.
Table of Contents
Genital herpes is a sexually transmitted infection (STI) that is spread by the herpes simplex virus. The herpes simplex virus (HSV) has two variants: HSV-1 and HSV-2. Each is equally capable of causing genital herpes, however HSV-2 is the commonly detected variant.
Genital herpes is spread through sexual contact with someone who has the virus. The virus can be passed without symptoms too. A person might not know they have it until it reappears or until they pass it on to their partner. People with genital herpes need to tell their partners about the infection before having sex so they don’t get infected.
Genital herpes causes include the presence of the herpes simplex virus (HSV). The first time someone contracts HSV, they have an outbreak. These outbreaks can recur periodically for people with a weakened immune system or who don’t take precautions to prevent an outbreak. Anyone who has ever had oral sex could contract genital herpes because HSV-1 can also cause it. But those with only one partner are at a lesser risk than those with multiple partners.
Condoms reduce the risk but do not completely eliminate it because condoms do not cover all areas where HSV may be present, such as in your mouth or fingers.
Genital herpes symptoms in men are as follows:
Genital herpes symptoms in women are as follows:
Some people with genital herpes may also experience atypical symptoms such as a fever, headache, and muscle aches.
Genital herpes is diagnosed by taking a swab from the affected area and sending it to a lab for testing. The swab will be examined for the presence of the herpes virus. A positive result indicates that you have genital herpes.
Two types of herpes simplex viruses – HSV-1 and HSV-2 – can cause oral or genital infection. The type detected determines whether the person has cold sores, fever blisters, or genital sores.

If you think you might have genital herpes, it’s important to see a doctor as soon as possible. Early diagnosis and treatment help prevent the virus from spreading and causing more serious health problems.
Your doctor will most likely be able to diagnose you based on your symptoms. They may also do a physical exam and swab your genitals for any signs of infection or disease. The test is easy, takes about 10 minutes, and can tell you if there are active HSV-1 or HSV-2 infections in your body.
No genital herpes cure exists at present but there are treatments that can help manage the symptoms. Antiviral medications can help bring down the number of outbreaks and make them less severe. In some cases, these medications can also help reduce the risk of transmitting the virus to others.
Following are the most common genital herpes treatments:
The most commonly prescribed medication is acyclovir (Zovirax). Studies have shown that Zovirax reduces the duration of a typical episode by about 24 hours when taken at the first sign of a tingling sensation or other signs of impending herpetic eruption.
Taking Zovirax daily may help lower the number of episodes for those who suffer from frequent recurrences.
Other ways to ease the discomfort of genital herpes include using ice packs and taking over-the-counter pain relievers like acetaminophen (Tylenol) or ibuprofen (Advil) during an episode.
Although cold compresses don’t provide any relief from itching, they can help prevent blistering during a herpes breakout by reducing blood flow to the affected area.
Though anyone can get genital herpes virus, some people are more susceptible and at greater risk:
These factors increase your chances of contracting HSV-2 and should be considered when discussing prevention methods.

If you suspect that you might have genital herpes, it’s important to see a doctor immediately. The CK Birla Hospital has a team of experienced doctors who can help you manage your condition and get the treatment you need. Your medical history will be taken, and an examination will be performed.
If an accurate diagnosis is made, you’ll receive information about other types of STD tests that should be conducted. After receiving this information, we recommend that you return for follow-up visits so that your progress can be monitored.
Contact us and book an appointment
Ques 1. Is genital herpes curable?
The answer is no. There is no cure for genital herpes, which means that once you’ve contracted it, you must live with it. However, there are many ways in which you can control your condition and make it less of an issue in your day-to-day life.
Ques 2. What triggers herpes genitalis?
HSV causes the herpes virus to appear on the skin or mucous membranes. To contract HSV, a person needs contact with someone who has the disease and contact with fluids from the infected person, such as saliva or semen.
Ques 3. What are the signs of herpes on a woman?
Women may experience sores on their vagina, vulva, cervix or anus; fever; nausea; muscle aches; headache; painful urination and vaginal discharge.
Ques 4. What are the stages of herpes?
HSV infection will either be dormant (no symptoms) or active (symptoms). If the infection becomes active, it will stay that way until treated. It takes about two weeks before there are noticeable symptoms but sometimes even longer. Once a person starts having outbreaks, they should expect one outbreak every 2-6 months if not treated properly.
Ques 5. Can a woman give a man herpes?
Yes, a woman can transmit herpes to her male partner through oral sex or unprotected sex because it’s possible for her to become infected with the virus during childbirth.
Pelvic pain can be very disruptive to your life, causing pain and discomfort during the day and night when you’re trying to sleep. But if you don’t treat it, you may develop long-term, chronic pelvic pain that never goes away and may even worsen over time.
Fortunately, there are ways to manage pelvic bone pain and even stop it from happening in the first place! Read on to learn more about the definition of pelvic pain , symptoms, causes, diagnosis, treatment, prevention, and more.
Table of Contents

Pelvic pain refers to pain in the lower abdomen, pelvis, or perineum—the area between the anus and vulva or scrotum. It can be for a short period or be a chronic long-term problem. Pelvic pain in women can affect them at any age, but it’s most common in women of childbearing age.
Following are some of the most common reasons for pelvic pain:
Other potential causes include:
In some cases, the cause of pelvic pain is unknown.
Pelvic pain can manifest in several ways, including a dull ache, sharp pain, or cramping. The pain may be constant or intermittent and can be exacerbated by activities like sitting for long periods, sexual intercourse, or urination.
In some cases, based on where pelvic pain is located, the pain may radiate to the lower back, thighs, or rectum.
Some other symptoms include the following:
There is no one definitive way to diagnose pelvic pain. Your doctor will likely start by taking your medical history and physical exam. They may also order imaging tests, such as an ultrasound or MRI, to get a better look at your pelvis.
In some cases, they may also recommend a laparoscopy, a minimally invasive surgery that allows them to look inside your pelvis. A laparoscopy can help detect endometriosis, ovarian cysts, fibroids, tumors, and other abnormalities in the uterus.
Most pelvic pain can be treated with a combination of physical therapy, medication, and lifestyle changes. In some cases, surgery may be necessary.
If you’re experiencing pelvic pain, there are a number of medications that can help.
Certain over-the-counter pain relievers such as ibuprofen and acetaminophen may help relieve mild discomfort from menstrual cramps or endometriosis.
For more severe pain, your doctor may prescribe other medicines like acetaminophen with codeine or hydrocodone with acetaminophen.
Sometimes, your doctor may also prescribe an antibiotic to fight infection. The most common type is Metronidazole, which treats bacterial vaginitis and sexually transmitted infections.
Two types of hormone treatments can be used to treat pelvic pain related to endometriosis, uterine fibroids, and hormonal birth control side effects: oral contraceptives and hormones delivered through a patch or injection into the skin.
Oral contraceptives work by altering hormone levels and reducing symptoms associated with menstruation while delivering estrogen directly into the bloodstream through pills taken daily.

Many women find relief from chronic pelvic pain through antidepressants. Selective serotonin reuptake inhibitors (SSRIs) are often prescribed when patients have depression or anxiety in addition to their chronic pelvic pain.
Many physical therapies may help treat pelvic pain. These include TENS, acupuncture, massage therapy, trigger point therapy, and more.
Psychotherapy is important when it comes to the management of chronic pain. Mindfulness-based stress reduction (MBSR) is another type of psychotherapy that has been shown to help alleviate chronic pain.
If medications fail to work, doctors might recommend spinal cord stimulation as an option. The procedure involves implanting an electrode near the spine that sends electrical impulses through the spinal cord, which blocks pain signals from reaching the brain.
It’s most effective for those with high levels of nerve damage and those who have tried all other options without success.
After performing a trigger point injection, patients usually notice relief from their pain within 24 hours.
To get the best results, injections should be performed at intervals of two weeks apart until symptoms lessen significantly.
For women with painful adhesions, laparoscopic surgery can be a good option. A small incision is made, and the surgeon inserts a lighted tube called a laparoscope into the pelvic cavity.
The laparoscope is connected to a camera, allowing the surgeon to see inside your body on a monitor screen.
Another treatment for pain caused by endometriosis is the surgical removal of the uterus (hysterectomy). Removing both ovaries may also help relieve pain caused by endometriosis.
It’s important to note that hysterectomies are not an effective treatment for endometriosis-related infertility. As with all surgeries, there’s always some risk involved, so you must discuss this procedure in detail with your doctor before going ahead with it.
If you’re experiencing pelvic pain, you can opt for pelvic pain home treatment female to help ease the discomfort.
First, take a warm bath or apply a heating pad to the area for 10-15 minutes. You can also try over-the-counter pain relievers like ibuprofen or acetaminophen. If the pain is caused by constipation, try eating more fibre-rich foods or taking a stool softener.
Finally, make sure you’re getting enough rest and staying hydrated.

If you’re experiencing pelvic pain, it’s important to see a doctor so they can determine the cause. In some cases, pelvic pain is caused by a minor issue and will go away on its own.
However, if the pain is severe or lasts more than a few days, you should see a doctor. They can run tests and rule out any serious causes of pelvic pain.
If you’re experiencing pelvic pain, the first step is to contact your doctor or a pelvic pain specialist. They will be able to help you determine the cause of your pain and the best course of treatment.
The CK Birla Hospital offers a comprehensive pelvic pain program that includes medical and surgical treatment options. We also offer a wide range of support services to help you cope with your pain and manage your symptoms. If you have any questions about pelvic pain, please don’t hesitate to contact us and book an appointment with Dr. Aruna Kalra.
Ovarian cysts, meaning follicular cysts, can cause pelvic or abdominal pain that can be quite severe. For many women, the pain is intermittent and will flare up every few months or so. Others experience constant and debilitating pain.
Most ovarian cysts are caused by a buildup of fluid in the ovaries. Other causes include:
While some ovarian cysts may not need any treatment, others may need to be removed surgically. If you have a high-risk type of follicular cyst called an endometrioma, it may need to be surgically removed because it might rupture, which could lead to internal bleeding.
There are a few key symptoms that can help you detect if you have ovarian cysts: one of them being lower back pain. Other symptoms include bloating, abnormal periods, infertility, and pelvic discomfort during intercourse.
Yes! Stress is one of the leading causes of both follicular cysts and functional cysts.
When there is a small tear in the mucosa, there lie moist tissues which line the anus and this is known as an anal fissure. Anal fissures may develop when the individual passes hard or large stools during the bowel movement. Anal fissures result in discomfort and bleeding during bowel movements. Additionally, there might be spasms at the end of the anus.
Anal fissures can affect persons of any age, but they are most frequent in newborns and infants. Most anal fissures improve with treatment like sits baths or increased fibre consumption. Anal fissure sufferers sometimes require medication or surgery.
Table of Contents
There are reasons that can cause anal fissures. Below are some of the common causes of anal fissures.
Other than the above mentioned, there are some causes that are not common.
You may be more susceptible to getting an anal fissure if you have the following factors:
Constipation: The danger of tear is increased by straining during bowel motions and passing firm stools.
Childbirth: There are times when post-delivery, women are more likely to develop anal fissures.
Age: Anal fissures can develop at any age, but they are more frequent in young children and middle-aged people.
Crohn’s illness: Crohn’s illness leads to chronic intestinal inflammation which may render the lining of the anal canal as it is more prone to wear and tear.
In addition to performing a physical examination that includes an examination of the anal region, your doctor will also ask about your medical history. This examination will help identify the root cause of the anal fissure and allow the doctor to plan to next course of action because the position of the fissure provides clues as to its cause. Instead of the rear or front of the anal hole, a fissure is more likely to be a symptom of another condition, like Crohn’s disease. If your doctor suspects an underlying issue, they might advise more testing:
Anoscopy: Tubular device inserted in the anus to allow your doctor to have a better vision of the rectum and anus.
Flexible sigmoidoscopy: Your doctor will insert a thin, flexible tube with a tiny video into the bottom portion of your colon.
Colonoscopy: Your doctor will insert a flexible tube into your rectum to inspect the entire colon. This test will help identify risk factors for colon cancer, signs of other conditions, or other symptoms such as abdominal pain or Diarrhoea.
As per diagnosis, below is the treatment plan for anal fissures.
If you are someone who suffers from severe constipation or Diarrhoea then it might not be possible to avoid anal fissures. Eating food high in fibre, and consuming a good quantity of fluids can help prevent or reduce the pain, itching and bleeding caused due to anal fissures. It is recommended to exercise regularly to be able to keep yourself away from frequent bowel movements.
Making necessary changes in your every routine can help relieve the discomfort and promote the healing process of anal fissures.
Boost your intake of fibre
Consuming 25 to 30 grams of fibre daily can keep stools soft and speed up the healing of fissures. Fruits, vegetables, nuts, and whole grains are examples of foods high in fibre.
Take fibre supplements
In order to avoid gas and bloating, gradually increase your consumption of fibre.
Drink enough water
Constipation can be avoided with fluids and for that, the easiest way is to consume at least 8-11 glasses of water every day.
When having a bowel movement, avoid struggling
Pressure from straining might produce a new tear or cause an existing tear to reopen.
Anal fissures usually take approximately 2 weeks to recover. Anal fissures can be back if the person frequently suffers from constipation or diarrhoea or is left untreated.
Untreated fissures might result in serious consequences. First off, delaying therapy can potentially delay a proper diagnosis because the state of the fissure deteriorates with each passing day. An incorrect diagnosis of an anal fissure may also cause other illnesses, like serious infections or even cancer, to go unnoticed and untreated.
Anal fissures take some time to heal. The doctor will prescribe certain medicines to relieve the pain and discomfort, suggest the patient consume food and vegetables rich in fibre content and increase the intake of fluids.
Thyroid disease is a medical problem that restricts your thyroid gland from producing the appropriate amount of hormones. Correctly, your thyroid produces the hormones necessary to keep your body operating normally. These thyroid hormones control how your body uses your energy. If you are feeling fatigued or there are some noticeable changes in your skin or hair then the doctor may conduct a physical exam and order blood tests to detect the functioning of the thyroid.
Post diagnosis, thyroid treatment depends on the type of thyroid and its underlying cause.
Dr. Abhay Ahluwalia, explains the types of thyroids, their symptoms, their causes, diagnosis and treatment.
Table of Contents
When the thyroid is unable to operate properly—either by releasing too much or not enough T4 hormone—thyroid illness develops. A lump or nodule may also form on your thyroid. Three primary thyroid conditions exist:
Hypothyroidism occurs when the thyroid gland does not produce enough T4 hormones. An underactive thyroid may occur because the pituitary gland, the hypothalamus, or the thyroid itself is not working properly. Nearly five per cent of the population has an underactive thyroid. More women than men suffer from the condition. Symptoms of an underactive thyroid include:
When the thyroid gland does not create enough Thyroxine (T4) hormone, hypothyroidism develops. Due to hypothyroidism, the pituitary, the hypothalamus, or the thyroid itself may not be functioning properly. The illness affects more women than men. Below are the symptoms associated with an underactive thyroid.
Hyperthyroidism occurs when the thyroid gland generates more thyroid hormones than the body requires. A malfunctioning brain, pituitary gland, or thyroid itself may produce an overactive thyroid. The cases of overactivity of the thyroid are not very common among people. Similar to an underactive thyroid, the disorder affects more women than men.
Symptoms of an overactive thyroid include:
When thyroid cells undergo changes and expand, malignant cells create nodules or growths, which is how thyroid cancer develops. These malignant nodules have the potential to migrate into the circulation, lymph nodes, and adjacent tissues if untreated. Though thyroid cancer is rare. However, over the years the cases of thyroid cancer have increased. There are four different kinds of thyroid cancer, papillary thyroid cancer, follicular thyroid cancer, medullary thyroid cancer and anaplastic thyroid cancer.
As per the symptoms, the patient visits the doctor to find the root cause of the disease. Based on the symptoms, the doctor is likely to perform a physical examination or diagnosis to assess and understand whether it is hypothyroidism or hyperthyroidism. Below are some tests done for the right analysis.
Levothyroxine (Synthroid®), a synthetic (man-made) thyroid hormone, is typically given to patients with hypothyroidism as this will help to restore the body’s hormone levels and will also relieve the symptoms. Periodically, your blood will be tested to make sure the medication given is successfully treating your hypothyroidism. The majority of patients with hypothyroidism require lifelong replacement thyroid hormone therapy.
The treatment for patients with overactive thyroid depends on how severe the symptoms are and what the underlying cause is. You and your doctor will discuss a few options as per each individual’s case. Medications like antithyroid medication, radioactive iodine, Beta-blockers and thyroidectomy (surgery).
Within six to twelve weeks of taking the medicine, symptoms normally start to go away, although therapy is routinely continued for at least a year. There are some side effects that are associated with the medicine, these antithyroid drugs may harm your liver and increase your susceptibility to infection and some people have allergic reactions to these drugs.
Many patients will require daily synthetic thyroid hormone to restore appropriate hormone levels in the body because radioactive iodine normally causes the thyroid to become underactive. Long-term use of radioactive iodine has demonstrated its safety.
Beta-blockers are used to lower high blood pressure. Although they do not directly treat the thyroid, beta blockers can help slow a fast heartbeat and avoid heart palpitations. In order to feel better until the thyroid is working more properly, patients are given beta blockers with anti-thyroid medicine and radioactive iodine. Beta-blockers are generally well tolerated by patients, however, some may have headaches, nausea, dizziness, or upset stomach.
A thyroidectomy, or surgical removal of the thyroid, is a treatment option for people who cannot use radioactive iodine or take antithyroid medication. The average surgery takes two to two and a half hours and after spending some time under observation, patients either go home that day or the following day. Although complications from thyroid surgery are uncommon, there is always a danger.
For thyroid cancer, surgery is the only treatment option. To remove the cancer cells, radioactive iodine therapy is employed. This applies to any remaining healthy tissue as well as any malignant cells. The doctor may remove neck lymph nodes for testing depending on the stage of the malignancy. Post-surgery, most patients may and will require daily synthetic thyroid hormone therapy for the rest of their lives. Your doctor and you will discuss your best surgical option based on the type of cancer you have and to what extent it has spread.
There have been several studies that indicate a relationship between thyroid and diabetes. Patients with thyroid disorder do have an increased risk of diabetes. Therefore, it is important to take care of the sugar levels.
Yes, thyroid issues i.e. severe hypothyroidism and hyperthyroidism can result in loss of hair. Once the treatment of thyroid starts it can take several months for the hair to grow back as it was before thyroid.
Feeling fatigued or tired goes away on its own with time. Doctors suggest taking all recommended medications on time and eating a diet that is healthy and full of nutrients.
Yes, there are several at-home thyroid test kits that can help diagnose thyroid disease.