Filter :
Piles, or hemorrhoid’s, are a globally relevant problem. These are swollen veins located inside your rectum, just outside the anus that is accompanied by pain, itching and in most cases bleeding. These can be managed with at-home treatments but sometimes requires medical intervention. With this blog, we will try and understand the problem better to be able to deal with it better.
Table of Contents
Piles are enlarged veins inside the rectum around the anal area. They are often swollen, painful, and uncomfortable and cause bleeding in the rectum. They are also called hemorrhoid’s. These are present in our body since birth, and only pose a problem when they become swollen and start irritating the rectal area.
Since it occurs due to a swollen vein, the type of hemorrhoid’s will depend upon the location. Broadly it is of 2 types:
Both these types can extend or bulge outside the rectal cavity, these are called prolapse hemorrhoid’s. However, it is different from an anal fissure, although they have similar symptoms. Anal fissures occur due to tissue rupture whereas this happens from swelling of veins.
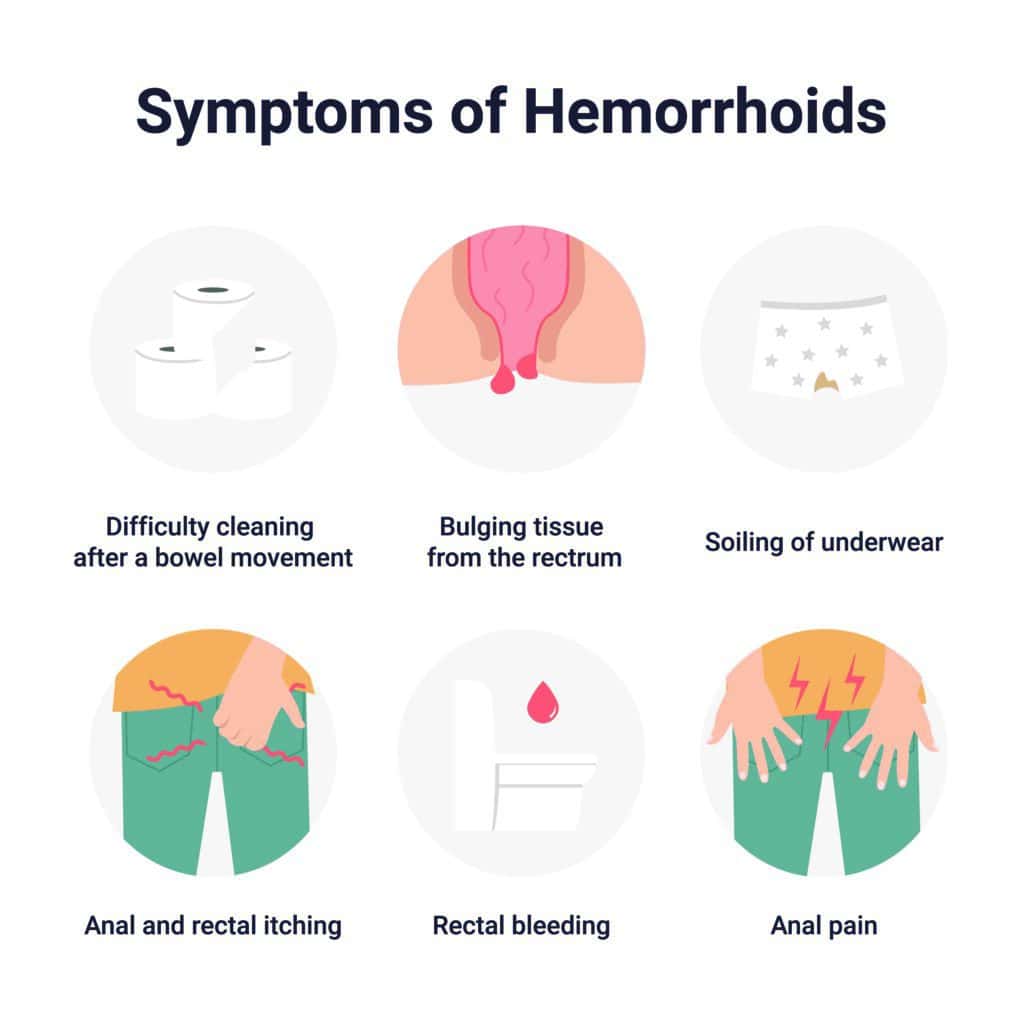
Symptoms of piles depend upon the type of piles. In the case of internal piles, one hardly has any symptoms, since there is hardly any pain in this case. One might find some blood during excretion, which is a sign of rectal bleeding.
The external or prolapsed piles will have clear symptoms. These include:
At this point, it is important to note that other conditions cause hemorrhoid’s-like symptoms, such as gastrointestinal disorders, bowel diseases, and in extreme cases colon cancer, Crohn’s disease, colitis, ulcer, etc.
It is advisable to be observant of any of the above symptoms. Be wary of abdominal pain or chronic constipation with rectal bleeding. If you notice any of these, reach out to a doctor for advice. The doctor will perform one or more of the following procedures to determine the root cause.
Based on the outcomes of these investigations, the next step will be a colonoscopy which will help detect any signs of colon cancer. These are all OPD procedures without anesthetic use. Therefore, there is nothing to be scared about.
Understanding a problem requires assessing the triggers that lead to the problem. Some of the relevant causes of piles or hemorrhoid’s are:
From these causes, we can understand the primary risk factors that may lead to piles over time. These are:
There are various ways in which piles can be handled. But broadly they can be categorized under home treatments and medical assistance from healthcare providers. Often in minor cases, piles heal without any treatment. If the symptoms surface, they usually last for a week.
At home, you can use over-the-counter medications over the affected area. Apart from this, you can:
If the above fails in relieving the pain, don’t lose sleep, reach out to a trusted healthcare provider and explain your situation clearly. Upon clear investigation and review of outcomes one of the following will be suggested:
Reach out to us in case you feel any of the symptoms above and seek medical attention from some of the best physicians in the field.
Piles are more common as we age. It can be prevented by maintaining a healthy lifestyle to avoid hard stools and constipation, which is the primary cause of piles.
Q1. How do Piles go away? Can Piles be cured permanently?
A. Sometimes piles can be cured by themselves without the person knowing they have piles. This happens in the case of internal piles where there is hardly any pain. For an external incident, over-the-counter ointments or the help of a medical practitioner will help treat the concern faster. With at-home remedies, piles can be managed but not cured completely. For that one needs to have surgical intervention.
Q2. How long do Piles take to heal?
A. The symptoms of piles last mostly for a week. If it goes away after seven days with over-the-counter medicine, then it has healed. If not, the help of a medical practitioner is required. Depending on the severity of the case and the stage of the piles the healing timeline will differ.
Q3. Can stress cause Piles?
A. By stress, if we mean putting pressure on the pelvic muscles, then yes. Apart from this, when we are mentally stressed out, our blood pressure is increased. In such a case also the existing condition of piles will worsen. Also, more stress leads to more consumption of alcohol, which in turn dehydrates the body, therefore worsening the piles.
Q4. What is the main cause of Piles?
A. The main cause of piles is constipation and improper bowel movements. If our stools are not soft and we spend hours in the washroom trying to pass them then it is a warning sign. The more pelvic pressure is applied the greater the chances of rectal bleeding. All of these are eventually the symptoms that show up in piles. So working at the root will help make things better, start by having a healthy diet rich in fibre that will assist in the process of passing stools.
Q5. What are the stages of Piles?
A. Medically internal piles have four grades:
It is normal for men to have occasional issues getting or keeping an erection. However, if the problem becomes more frequent, then it is recommended to visit a doctor as soon as possible.
Erectile dysfunction problems might persist because of underlying health or emotional and relationship issues. The sooner you get yourself checked, the better it would be to treat the condition.
Table of Contents
Erectile Dysfunction (ED) refers to the inability to get or maintain a penile erection for sexual intercourse. In earlier days, ED was also referred to as impotence.
Without proper diagnosis and treatment, it can be difficult for an individual to cure erectile dysfunction. Further, ED in men over 40 is a major warning of cardiovascular conditions.
Erectile dysfunction can be diagnosed in males across all age groups. However, it is slightly more common in men in their late 40s and early 50s.
The following symptoms suggest erectile dysfunction in men:
Men can experience erectile dysfunction due to health problems or sometimes due to underlying and undiscovered emotional troubles:
Once you visit a Male Sexual Dysfunction doctor regarding your erectile problems, they will ask you questions about your medical history and order some physical tests to better understand your situation.
These physical tests will help diagnose the real cause of your situation or any other probable underlying health problems. Additionally, some routine medical tests will also be carried out like urine tests, blood tests, thyroid tests, etc.
An ultrasound will help determine if there is any problem with the flow of blood into the penis.
An erection is the result of increased blood flow into the penis. Sexual thoughts and foreplay before sexual intercourse stimulate the blood flow.
Hence, if the blood is not flowing into the penis properly and the penis fails to become erect during sexual activities, it can be determined through an ultrasound.
A medicated drug is inserted into the penis during the injection test to stimulate an erection. Once the penis is erect, the doctor will check the firmness and how long does the erection last.
This test is often combined with other physical exams like ultrasound and urine tests to give the doctor a proper overview of erectile dysfunction.
A nocturnal penile tumescence test (NPT) is performed to analyse erections during sleep.
It is common for men to have 3-4 erections during a normal cycle of deep sleep. To check the erections, an electrical device is worn on the thigh to store data.
The data is then accessed later by the doctor to make a diagnosis.
Dealing with erectile dysfunction can be emotionally and mentally draining. It is completely normal to have numerous doubts and queries in your mind.
Here are some common questions about ED that you can ask during doctor consultations:
The treatment for erectile dysfunction starts with making some lifestyle changes and taking care of your cardiovascular health.
Some erectile issues can be treated by small changes like losing weight, doing erectile dysfunction exercises, avoiding alcohol/smoking, relieving stress, etc.
Apart from the lifestyle changes, your doctor will begin by suggesting some non-invasive medical treatments. These are known to have worked effectively and safely:
You might experience some side effects like headache, indigestion, facial flushing, stuffy nose, or muscle pain after taking oral medication. However, do not be alarmed as these side effects are only short-lived and mild.
Erectile dysfunction is not only caused due to health problems but also emotional issues.
Emotional stress or relationship anxiety can creep into your mind while performing sexual activities, making it difficult for you to experience pleasure out of it.
However, psychological treatment options like counselling sessions with a trained counsellor can help you address your emotional issues and needs.
Sex therapy has also proved to be beneficial for many men. A skilled sex therapist can help you identify your sexual needs and how to effectively communicate with your partner regarding the same.
Penile implants are one of the major surgical treatment options available for treating erectile dysfunction.
Penile implants, also referred to as penile prostheses, are placed inside the male reproductive organ to stimulate an erect penis during sexual intimacy and intercourse.
However, this surgical treatment is not advisable for ageing men. Their options are limited to medical and therapeutic erectile dysfunction treatments.
There are two kinds of penile implants, namely, semi-rigid implants and inflatable implants.
The semi-rigid implant is made using silicone, which gives firmness during sexual penetration and can be easily bent downward and upward during peeing.
The inflatable implant, on the other hand, is inflated through a pump placed inside the scrotum. When the pump is engaged during sexual activity, the penis inflates and becomes erect. Using the pump in the scrotum, men can easily manage the firmness and size of the erection.
Taking action is crucial if you notice erectile dysfunction problems more than 50% of the time in your overall sexual activities.
While it might be embarrassing to communicate about this issue, do not hesitate to reach out for help. A professional will not only help you diagnose and treat the condition but will also respect your privacy by keeping all the information confidential.
Visit the CK Birla Hospital(R) or book an appointment with Dr. Shalabh Agrawal to learn more about your condition and get the best treatment for erectile dysfunction.
#1 How can you fix your erectile dysfunction?
Erectile dysfunction can be treated through several medical, surgical, and psychological treatments.
Medical treatments include solutions like penile injections and testosterone therapy. The penile implant option is available for surgical treatments, depending on factors like age and medical history.
#2 Can erectile dysfunction get cured?
Yes, erectile dysfunction can be cured through several medical and psychological treatments.
The situation can also be improved by making some lifestyle changes like avoiding alcohol, exercising regularly, improving cardiovascular health, etc.
#3 How can I test for erectile dysfunction at home?
It is not advisable to indulge in self-testing for erectile dysfunction at home.
You can visit a doctor to seek professional diagnosis and treatment. A doctor can conduct physical exams to understand your situation better.
#4 What is the main cause of erectile dysfunction?
Some of the main causes of erectile dysfunction are underlying health problems like cardiovascular diseases, obesity, high blood pressure, etc.
Erectile dysfunction is often also caused due to emotional issues also like anxiety, stress, and low self-esteem.
Table of Contents
Usually caused by severe head injuries, a subdural hematoma (SDH) refers to the collection of blood inside the head but outside the actual brain tissue. Bleeding occurs between the brain’s outermost layer, known as dura, and the next layer, the arachnoid.
Resulting from tears in the bridging veins, a subdural hematoma causes increased pressure on the skull, leading to damage to the brain tissue. If the pressure rises to a very high level, it can be life-threatening and lead to death.
Subdural hematoma is classified into different types based on the amount of bleeding, the speed of its development, and the damage it causes. Following are the different types of SDH:
The following are at risk of suffering from a subdural hematoma:
Subdural hematoma symptoms include the following:
Severe cases of subdural hematoma show the following symptoms:
Your healthcare provider will perform a thorough physical examination by checking your blood pressure and heart rate, examining your eyes, and looking for any other signs of bleeding.
They will also ask you about any previous diseases, the medications you are on, the history of any injury, etc. Sometimes you may need to get an angiography to check for any bleeding in the vessels of the brain.
Besides that, they may order a CT scan and MRI of the skull and brain to locate the bleeding. They can then prescribe some blood tests to understand if there has been any blood loss indicating the presence of a subdural hematoma.
The choice of treatment for a subdural bleed depends on the size and location of the bleeding and the patient’s symptoms.
Typically, those suffering from a subdural haemorrhage need hospitalisation, life support care, and surgical management. However, some hematomas are very small, and the body can absorb those with the help of non-surgical measures.
A brain hematoma can cause complications depending on its size and location, the individual’s age and overall health, the severity of the injury, and some medications that may delay the healing procedure.
Seizures, permanent loss of muscle strength, brain herniation, and chronic numbness are some complications arising from subdural hematomas.
An extensive bleed or subdural hematoma bilateral can cause too much pressure on the brain and may lead to coma or even death.
The prevention of a brain haemorrhage is targeted at eliminating the causative factors. Some types of hematomas may not be prevented; however, you can take measures to at least reduce the risk.
Since subdural hematomas are life-threatening, they need to be prevented. If you develop them somehow, you need immediate treatment.
The CK Birla Hospital(R) is a leading healthcare institution that offers subdural hematoma treatment at all our state-of-art facilities. We have a qualified neurosurgery department with the latest facilities and technologies to manage these cases, along with the expertise of doctors who have conducted numerous surgeries.
Visit the CK Birla Hospital(R) or book an appointment with Dr. Rajeev Gupta
Some patients with a subdural hematoma may recover in a few weeks or months, while others don’t recover even after years.
A subdural bleed primarily requires a craniotomy, a surgical treatment.
About 50% of patients survive after a subdural haemorrhage, though permanent brain damage may occur after it has been experienced.
Depending on the location, size, and severity of the subdural hematoma, it may subside completely in a few months, or the residual effect may last for a long time.
Sometimes, small subdural hematomas can be managed non-surgically with regular monitoring.
Tendons are the fibrous tissues that connect the body’s muscles to the bones.
Tendons are very flexible and allow us to move our limbs in all directions. The human body contains over a thousand tendons from head to toe. They vary in shape and size depending on where they are in the body.
Tendons also save the bones and muscles from injury by absorbing most of the impact. Additionally, when a body is engaged in physical activities like running, jumping, climbing, etc., the tendons stretch flexibly with the muscles making the movements smoother.
Table of Contents
Tendonitis, also referred to as tendinitis or tendinopathy, is the inflammation and irritation of the tendon. Depending on the degree of tendonitis, the pain and tenderness caused by it can vary.
Anyone, irrespective of age and gender, can get tendonitis while doing strenuous activities and even some common everyday activities like gardening, bathing, playing, etc. Sometimes, maintaining an incorrect posture for extended durations can also trigger this condition.
Tendonitis and tendinosis are often confused with each other. While these conditions have similar causes and symptoms, tendinosis refers to chronic tendonitis. With time, tendinosis can become more serious and extremely difficult to treat.
Depending on the seriousness of the tendon injury, the symptoms can vary. However, some common tendonitis symptoms are:
Some of the common causes of tendonitis are:
Depending upon which tendon of the body has been affected, tendonitis can be majorly divided into 5 types:
Achilles tendonitis affects the Achilles tendon, which connects the heel bone to the calf muscles. It is a very common sports injury caused due to extensive strain on the calf muscles. With proper care, it can be treated in 1-2 weeks.
The inflammation and irritation in the supraspinatus tendon lead to supraspinatus tendonitis or shoulder tendonitis.
The supraspinatus tendon is in the shoulder and is one of the common locations of tendon rupture. Repetitive strenuous activities and ageing are two of its main causes.
The wrist tendons connect the muscles in the forearms to the bones in the hand. There are a total of 6 tendons here that control the movements of the wrist, hand, and finger.
Lifting heavy loads for long hours and impactful injury can cause wrist tendonitis.
In trigger finger tendonitis, the tendon surrounding the finger becomes inflamed, keeping the finger locked in a bent position. It can be painful and highly inconvenient.
It is also referred to as tennis elbow or lateral epicondylitis. In this condition, a person experiences pain they bend the elbow outwards. If left untreated for a long, the pain can travel to the shoulders and wrist.
Usually, minor tendonitis injuries can heal with 3-4 days of rest. However, if your pain does not go away, visit a doctor as soon as possible.
Neglecting persistent tendonitis pain can lead to the development of chronic tendonitis. A proper diagnosis will allow you to know the extent of your injury and take steps for treatment accordingly.
When you visit the doctor, they will ask you to explain how you got the injury. Make sure you provide all the information to the doctor as accurately as possible. They might also ask you about your medical history to devise an informed treatment plan.
The doctor might recommend some physical exams such as X-rays and joint aspiration. To take X-rays, radiation is used to create a scan of your tendons, allowing the doctor to catch internal injuries. In joint aspiration, a needle is inserted neat the inflamed tendon to collect fluid from the joint and check it for infections.
Some of the common treatment plans for tendonitis are:
There are some simple steps you can follow to prevent tendonitis:
It’s crucial to visit a doctor if your tendonitis symptoms are not going away even after resting for a week or two. Make sure you reach out to a specialist orthopedic since identifying the pain point will be crucial. If you are struggling with tendonitis, you can always reach out to our Department of Orthopedics at the CK Birla Hospital(R) or book an appointment with Dr. Anuj Chawla
How long will recovery from tendonitis take?
You can recover from tendonitis if you get proper rest for one or two weeks. You can also take other measures, like hot/cold compression, pain medication, etc., to help you recover faster. However, if the pain persists, visit a doctor as soon as possible.
What triggers tendonitis?
Prolonged strenuous physical exercises can trigger tendonitis. Some other factors, like ageing, diabetes, rheumatoid arthritis, etc., can also contribute to tendonitis.
What can a doctor do for tendonitis?
Depending on the severity of the tendonitis, the treatment your doctor recommends might vary. They may administer pain medicines to minimise discomfort. Sometimes physical therapy is also recommended to treat severe tendonitis.
Does tendonitis go away on its own?
You may recover from tendonitis with proper rest for a week or two. However, if your symptoms do not improve, we recommend visiting a doctor as soon as possible.
Many men with fertility problems and reduced semen quality are diagnosed with varicocele, an enlargement of the veins in the scrotum.
This potentially painful condition can cause infertility, so it’s important to understand what symptoms you may experience and why your varicocele was diagnosed in the first place.
Table of Contents
Varicocele is a condition that affects the veins in the scrotum.
The scrotum is the sac that holds the testicles. The veins in the scrotum are responsible for carrying blood away from the testicles. When these veins become enlarged, it’s called varicocele.
Many people with varicoceles do not experience any symptoms. However, when present, symptoms may include pain or discomfort in the testicle area (less common), low-grade fever (less common), and a general feeling of heaviness or discomfort in the scrotum (more common).
In some cases, there may be tenderness on one side of the scrotum due to blockage of venous drainage by an enlarged vein on that side of the body.
The exact varicocele causes are unknown. However, it’s thought that they may be caused by abnormal development of the veins in the testicles. This can happen during fetal development or after puberty.
In some cases, varicoceles may be caused by an injury to the testicles. Other possible causes include a clotting disorder or testicular torsion (when the testicle twists within its protective sac).
Men who have a history of kidney stones should also talk with their doctor about the risk for this condition.
If a man has had one episode of kidney stones, he has a 15% chance of developing them again. For men who have had two episodes, the likelihood increases to 30%.
Kidney stones are more common among men because they produce less urine than women. Therefore, there is more concentrated urine sitting in the bladder and collecting bacteria than would otherwise be present if there were more frequent urination as with women.
The most common varicocele symptom is a dull ache in the testicle on the affected side. The testicular pain may worsen with prolonged standing or sitting.
Other symptoms may include:
It’s important to see a doctor even if you don’t have any symptoms because varicoceles can lead to serious complications later on.
The scrotum will be visually inspected and touched to assess the possibility of a varicocele. The examination is typically conducted while you’re standing and while you’re lying down.
As you stand, your health care provider may ask you to take a deep breath, hold it and bear down, similar to how you do during a bowel movement. The Valsalva maneuver can make examining a varicocele easier.
A few different varicocele treatments are available, depending on the severity of the condition.
In some cases, no treatment is necessary. For milder cases, treatment may involve wearing special support stockings or taking over-the-counter pain relievers. For more severe cases, surgery may be necessary to remove the varicocele.
Doctors might sometimes recommend a surgery called varicocelectomy. A surgeon makes an incision in the groin area and removes one or both of the enlarged veins that are causing the problem.
If only one vein is removed, it’s typically done by ligation (tying off) because removing it surgically can lead to complications such as bleeding or scarring. If both veins are removed, they’re usually tied off so they can heal before removal from circulation.
One type of surgery used to correct varicoceles is laparoscopic varicocelectomy. Doctors insert a small tube with a camera attached through an incision near the navel and make another incision near the testicles.
They then cut away excess tissue from inside the scrotum and repair any abnormal connections between arteries and veins. Afterwards, surgeons seal off each end of the abnormal vessel connections using heat-activated clamps known as sutures.
Another procedure performed to stop blood flow coming from the varicocele is percutaneous embolization. With this technique, doctors inject tiny particles into the larger veins that supply blood to the varicocele.
The particles block blood flow, and pressure in the vessels decreases until they shrink away completely. Endovascular procedures have been found to have higher success rates than other types of treatments, but there are still risks involved with these techniques.
In most cases, the varicocele surgery can be done on an outpatient basis, which means you won’t have to stay in the hospital overnight. Recovery from the surgery is usually quick, and you can expect to return to normal activities within a week or so.
However, there are some possible side effects of surgery that you should be aware of before deciding whether or not to undergo this procedure.
For example, a low sperm count might result from removing the affected veins, although it’s rare for it to happen with just one operation.
Additionally, if you’re not completely cured after one operation (which happens in about 5% of cases), then additional procedures might be necessary down the line.
Varicoceles are often harmless and don’t require treatment. However, in some cases, they can cause fertility problems. They may also increase the risk of testicular torsion (twisting of the spermatic cord) or testicular rupture.
Surgery is sometimes recommended for men who want to conceive a child but have varicoceles. If surgery is not an option, the male partner should avoid contact sports or any activity that might lead to trauma during sex.
The female partner should undergo tests to ensure she doesn’t have a condition like pelvic inflammatory disease that would make it more difficult for her to get pregnant.
Both partners will need regular checkups as well as consultation with specialists in reproductive medicine.
If you are experiencing any varicocele symptoms, visit the CK Birla Hospital or book an appointment with .We will help you develop a treatment plan that is best suited for your condition, besides providing you with information on the causes and symptoms of varicoceles.
Can Varicocele be Cured?
Treatment for varicocele includes surgery to remove the swollen veins that are in the scrotum. Other treatment options include injecting certain drugs to destroy the enlarged veins or radiation therapy.
What happens if a Varicocele is left Untreated?
If left untreated, the varicocele may cause infertility in men due to damage to the spermatic cord and blood vessels by persistent pressure on them. It also may lead to chronic pain, swelling and lower back pain.
Can Varicoceles disappear naturally?
Rarely, but it could happen over time as the body compensates.
Most of the time, this condition doesn’t go away without treatment and will get worse over time. Not only do the varicose veins become more dilated, but there is an increase in the connective tissue around the veins, which does not allow them to return to their normal size.
What is the natural way to Cure Varicocele?
There is no natural way to cure varicocele. However, preventive methods include wearing supportive underwear and avoiding high-intensity exercises like biking, running, weightlifting or heavy lifting.
Spinal stenosis is a medical condition in which pressure on the spinal nerves causes various symptoms, including muscle weakness, numbness and tingling, leg pain, and back pain. Most often, the symptoms are low back pain and leg pain that worsens with activity.
The spinal cord is located within the bony spine (spinal column) and carries messages between the brain and body. Nerves branch out from the spinal cord to bring these messages to various parts of your body.
The spinal canal is a hollow space that runs through your spine. It protects your spinal cord and nerves. Too much pressure on the spinal cord or nerves can cause problems with movement and sensation (called neuropathy). If there’s too much pressure on the nerves in your back, it may also cause pain.
Table of Contents
If you have spinal stenosis, you may have trouble moving your legs or arms and lose strength or stamina when walking or climbing stairs. You may feel like something is pulling on one side of your body when you bend over.
The symptoms of spinal stenosis can vary depending on where they are located in the spine:
Further, the symptoms may vary from person to person but commonly include:
The causes of spinal stenosis can be divided into two categories:

The most common cause of herniated discs is ageing, which can also happen after a back injury or a fall. You may have one or more discs in your spine affected by this problem.
The bulging disc puts pressure on the nerves that travel through your spine and cause pain and weakness in your legs and arms.
Spinal stenosis also occurs due to abnormal narrowing (stenosis) of one or more spaces within the spinal canal that contain spinal nerves or spinal discs, resulting in pressure on these structures.
The bones forming this area may be abnormally shaped or misshapen, causing them to rub against each other as you move.
The following risk factors may increase your chances of developing spinal stenosis:
Spinal stenosis is diagnosed based on your signs and symptoms, imaging tests and sometimes a physical examination, which will check for tenderness in the lower back and thighs, leg strength and reflexes.
Your Spinal Stenosis doctor may use one or a combination of these tests to help diagnose your condition:
These are the most recommended options for spinal stenosis treatment:
This option is usually considered when pain has not responded to conservative treatment. The goal of surgery is to remove the narrow portion of bone or tissue that is compressing the nerve root.
Possible surgical treatments include:
Steroids are often injected into the spinal canal to reduce inflammation in people with spinal stenosis who do not respond to medications or want faster relief from symptoms.
Steroids may be injected directly into the spinal canal, which relieves pressure on the nerves inside it, or into the epidural space between the bones of your spine and your dura mater (the outermost layer of your spinal cord).
Epidural steroid injections usually have few side effects but can sometimes cause bleeding or infection at the injection site, as well as headaches and dizziness — especially when standing up quickly.
Recovery from spinal stenosis surgery usually takes two to three months. The length of time it takes to recover varies from person to person and depends on many factors, including age, health, and duration of symptoms.
You will have to avoid strenuous activity and heavy lifting during this period. The first three to four days after surgery are the most critical, so your doctor may request you to stay in the hospital during this time.
The pain from spinal stenosis can be mild to severe and debilitating. It is important to visit a doctor and get a check-up to explore your treatment options. Visit the C.K Birla hospital near you or book an appointment with for a consultation.
1. Where does spinal stenosis occur?
Spinal stenosis occurs most often in the lower (lumbar) spine. It can also occur in the neck (cervical).
2. Who gets spinal stenosis?
Spinal stenosis most often affects people over age 50, although it can occur at any age.
3. Can spinal stenosis cause permanent paralysis?
The answer to this question is both yes and no. Some patients with spinal stenosis may present with permanent paralysis. However, in most cases, the paralysis is temporary, lasting for a few weeks or months.
4. When is spinal stenosis surgery considered?
Surgical treatment of spinal stenosis is usually recommended for patients who have pain and other symptoms that affect their daily activities. Surgery may also be used to relieve compression on nerves in cases where there is no improvement with nonsurgical treatments.
5. Is spinal surgery safe?
In rare cases, surgery is not considered safe because of other medical conditions or because the patient might be too frail from age or illness to tolerate the procedure well.
You may also be recommended not to have surgery if you have cancer or another serious condition that could be worsened by the procedure.
Gout is a painful arthritis condition that results in pain, tenderness, and inflammation in the joints. It can happen to anyone and at any time. While gout pain is generally felt in the hallux or the big toe, it can affect other areas too. Its vital to understand the implications of gout in more detail to identify and tackle this disease in a timely and efficient way.
Table of Contents
Gout is caused by excess uric acid in the body. Uric acid results from the breakdown of purines, which are naturally present in the body and also found in certain foods. The body generally removes the excess uric acid via the kidneys. The issue arises when the body fails to maintain the required levels of uric acid by either producing too much or failing to eliminate the excess quantity.

When uric acid levels become too high, sharp and hard crystals begin to form and deposit in various joints. You may not even be aware of this build-up happening over time.
Gout disease can present various symptoms, which can also vary in severity. The symptoms can feel quite severe during the flare phase of the disease. On the other hand, during the remission phase, you may not experience any symptoms at all.

Some of the most prevalent gout symptoms during an attack are:
Certain risk factors make you more vulnerable to hyperuricemia, or high uric acid, which in turn could lead to gout disease. Here are the ones to be aware of:

It’s worth noting that not everybody with high uric acid levels will experience gout.
If you’ve been feeling sudden and intense joint pain, it’s time to visit your general physician or rheumatologist for a consultation. You should share your symptoms in detail with your doctor, who’ll examine the affected joint and may order the following tests to diagnose gout:

Once your doctor has confirmed a gout diagnosis, the next step is to devise a suitable treatment plan.
There are two types of medications used for gout treatment. While certain medicines are advised to manage the pain and inflammation symptoms of gout, other medicines may be prescribed to reduce the uric acid levels in the body.
You must take medicines under the supervision of your doctor. Work with them to outline a treatment plan that works for your specific case.
Seeking timely treatment for gout disease is essential. If not treated, the frequency of gout flares can increase, and the disease may even start affecting other joints. Continuous gout attacks can deteriorate your arthritis over time (known as gouty arthritis). From cardiovascular problems to joint erosion, there can be many harmful consequences.

If uric acid levels continue to remain high, the crystals may start building up in the urinary tract as well, thus leading to kidney stones. As gout disease worsens and reaches the advanced stage, you may develop tophi, which are hard deposits of the uric acid crystals under the skin. Tophi can form in heels, toes, knees, elbows, fingers, etc. Even though tophi aren’t painful, they can disrupt daily activities and damage joints.
Gout attacks can feel debilitating and hamper many aspects of your life. However, through diet and lifestyle improvements, you can bring the disease as well as its negative impact under control. Here are some effective practices and remedies for gout pain that you can adopt:

While gout is an incurable condition, there are many ways to manage it to promote healthy living. Through medicines and self-care, you can minimise the impact of the disease on your life. Not only is it possible to reduce the frequency of gout attacks, but it’s also possible to reduce the pain and intensity of these attacks.
If you or someone you know is struggling with gout, then visit the nearest CK Birla Hospital or book your appointment with Dr. Rakesh Mattoo to get the best gout treatment and care.
Q 1. When should I see a doctor for gout?
A. If you’ve been experiencing symptoms commonly associated with gout, you should see your doctor immediately. In case there’s another medical issue causing the gout-like symptoms, like a joint infection, you want to get ahead of that promptly.
Q 2. How can I get quick relief from a painful gout attack?
A. Some quick remedies for gout pain include elevation of the impacted area and application of an ice pack. Talk to your doctor about medication for pain relief.
Q 3. What are some common warning signs of gout to watch out for?
A. If you feel severe joint pain (especially at night) that is sudden and extreme at the beginning and subsides after a few hours, it could be a sign of gout. Your joint is also likely to feel tender to even the slightest touch.
Q 4. How long does a gout attack last?
A. A typical gout attack can affect you for 1-2 weeks. The pain is worst during the first few hours of the attack. Treatment can help reduce the duration.
Q 5. What are some of the foods to avoid with gout?
A. Drinks and foods to avoid with gout include alcohol, organ meats, red meats, some seafood like sardines and scallops, fructose-rich products, etc.
The kidneys are located on either side of your spine in the lower back region. They are bean-shaped organs and filter the waste products from your blood. They also produce vital hormones and balance crucial elements in your body like calcium, potassium, and sodium.
The proper functioning of your kidneys is critical to your health. You need to be aware of signs that there might be something wrong with your kidneys in the case of renal failure.
Table of Contents
There are two types of renal failure – acute renal failure or acute kidney injury (AKI) and chronic kidney disease (CKD).
AKI occurs suddenly, accompanied by acute pain. On the other hand, the symptoms of CKD appear gradually, and you may not realise it initially.
AKI occurs as soon as the kidney abruptly stops functioning normally. Renal failure symptoms of AKI are:
CKD advances slowly and reveals little or no symptoms in the early stages. You may not feel much until your kidney function reduces to 20% or less.
By this time, the following renal failure symptoms might appear:
Also Read: Healthy Diet Chart for High Blood Pressure Patients
The most common causes of renal failure are uncontrolled high blood pressure and diabetes, among other reasons.
If your kidneys suddenly deteriorate, your kidney disorder would come under the category of acute kidney injury.
You can suffer this type of renal failure due to the following:
Renal failure diagnosis is performed by observing how the kidneys are filtering impurities in the body. The filtering function of the kidneys is facilitated by tiny blood vessels called ‘glomeruli.’
To measure the rate of blood filtration by the glomeruli, the glomerular filtration rate (GFR) readings are taken.

A normally-functioning kidney typically should filter blood at 100 millilitres per minute. The value fluctuates with age and gender. Certain formulae, considering age and gender, are applied to get accurate and relevant GFR readings.
Another means of detecting renal failure is to check the creatinine levels through a blood test. Creatinine is a waste product that is excreted through urine. High creatinine levels in the blood indicate malfunctioning kidneys.
You cannot prevent chronic kidney disease. However, if you are diagnosed with renal failure, there is much you can do to restore your kidney function.
Suppose you adopt a healthy lifestyle and take certain preventive measures to manage renal failure. In that case, you can slow down the deterioration of your kidney function by observing the following:
Renal failure treatment depends on the extent of the condition. If you receive timely treatment for chronic kidney disease, you can delay the progression of the disease.
One or multiple measures may be required for proper management of renal failure.
Your doctor appointments might include routine blood pressure checks and blood tests. You will also receive a regime of medication that you should follow strictly post-renal failure.
In case of complete renal failure, you will probably have to undergo dialysis regularly. Dialysis is a process where your blood gets filtered by a machine that does the job of your kidneys.

Alternatively, kidney transplant surgery is an extreme but effective method used by doctors to deal with the complications of renal failure. A kidney transplant operation involves replacing a defective kidney with the healthy one of a deceased or living donor.
If you start to experience any of the renal failure symptoms mentioned above, waste no time visiting a doctor.
When renal failure occurs, it can happen suddenly or gradually. If you get help immediately, you can arrest the progress of your medical condition. You don’t want to reach a stage where you will need dialysis.
To avail of expert advice and treatment, visit the C. K. Birla hospital or book an appointment with Dr Abhay Ahluwalia, who will recommend the best line of renal failure treatment for you.
With renal failure, you may experience swelling in your hands and feet. You may feel tired because your blood isn’t getting purified as well as it should.
If your kidneys stop functioning altogether, your doctor will recommend dialysis. Extreme cases will call for kidney transplant surgery.
If your kidneys stop functioning normally, your urine will appear dark brown due to excessive waste. You may find that you need to urinate less frequently. You might also observe foaming in your urine.
This is caused by increased protein levels in the urine. Increased protein in the urine is a sure sign of malfunctioning kidneys.
There are multiple causes of renal failure, but the leading cause is diabetes. Uncontrolled blood pressure can also take a toll on the kidneys.
Kidney disease, hereditary or otherwise, can also cause renal failure. Besides that, it can also stem from urinary tract issues, an enlarged prostate, kidney stones and various types of cancers.
All types of renal failure are serious and should be dealt with immediately. In extreme cases, it can be fatal. However, if you take timely action, you can reverse the effects of kidney failure, especially in the case of acute kidney injury (AKI).
There is no fixed formula for kidney failure recovery. However, if you are healthy and relatively young, the prognosis for total recovery can be good.
On the other hand, if you have comorbidities (existing medical conditions), there could be multiple complications of renal failure. The line of treatment would be more complex and extensive. Full recovery in such a case can prove to be more challenging.
The three early signs of renal disease are as follows:
Abdominal pain in children is a common complaint. It can be caused by various conditions, including constipation, gas, indigestion, abdominal muscle strain, and infections.
Sometimes, the cause is not apparent even after tests are done. In these cases, it’s essential to find out what’s causing your child’s symptoms so you can help your child feel better as quickly as possible.
Children can experience pain in the right lower abdomen to the upper abdomen and sometimes even as far as the chest (although this is rare). This type of pain can be:
Table of Contents
Common symptoms of children’s abdominal pain include:
The best way to help your child explain their pain symptoms is to discuss them. It’s vital for you and your child to understand the problem so you can discuss it with your doctor, who can devise a treatment plan.
Discussing pain with children can be challenging because they often don’t know how to describe their feelings. The following tips may help:
If your child is younger than six months old, contact a doctor right away if their belly looks swollen or distended (like a balloon being blown up). This could be from an intestinal blockage or other serious problem.
If your child is six months or older, call the doctor if:
These symptoms may be signs of appendicitis.
As a rule of thumb, you should see your doctor if your child:
A doctor diagnoses abdominal pain in children and babies after a thorough physical examination, history and investigations.
Diagnosing abdominal pain starts with a medical history and physical examination. Your doctor will inquire about the timing and location of the pain and how long it lasts.
They’ll ask questions about recent nausea, vomiting or diarrhoea your child has experienced. Your doctor will also examine your child’s abdomen to look for signs indicating an underlying problem.
Paediatricians use special techniques to pinpoint the cause of stomach pain in children. Some of these techniques include:
The most common cause of abdominal pain in children is a viral infection. The pain can be severe and usually go away in a few days.
If your child has pain in the lower abdomen, here’s what to do:
Abdominal pain is a common problem among children, and multiple potential causes of acute, recurrent, or chronic abdominal pain exist.
If your child complains of abdominal pain unrelated to food poisoning or constipation, consult a pediatrician at the CK Birla Hospital, or book an appointment with Dr Anukalp Prakash to learn more about treatment options.
It’s essential to understand the different types of lower abdominal pain in children and what they mean so that you can determine if your child needs urgent medical care.
Ask them the following questions:
Tummy aches are common in children. It’s essential to watch for signs (like a fever) that could signal a more serious problem and get help if needed.
If you don’t know when the fever started or how high it got (or if it came on suddenly), call your doctor immediately since it might be an infection that needs treatment.