Filter :
Did you know the medical term for menstrual cramps is “Dysmenorrhea”? Almost every woman can vouch to have experienced menstrual cramps severe enough to need medication. In reality, periods may be a permanent part of our lives, the severe pain associated with periods, on the other hand, need not be. The lack of awareness added to the social stigma associated with menstruation contributes to millions of women suffering silently from period pain. In this article, Dr Anjali Kumar, reputed obstetrician and gynaecologist in Delhi NCR talks about painful periods, its possible causes and preventive measures.
Table of Contents
Before we understand why periods can cause extreme pain in some women, let us understand what happens in the body during this process.
Every month, the female body prepares itself for pregnancy by building up the uterine lining. When the matured egg released by the ovaries every month is not fertilised, the body starts shedding this excess uterine lining resulting in “periods”. In order to push out the excess lining from the vagina, the uterine muscles contract and relax. This may result in severe muscle cramps for some women, and be barely noticeable in others.
Period pain need not be limited to the abdomen, it can also manifest as pain in the back, legs, thighs etc. It can also cause nausea, vomiting and diarrhoea.
Did you know that there are two different types of period pain? Doctors classify dysmenorrhoea (period pain) into two main categories:
Primary dysmenorrhoea is pain that is mainly caused by the uterine muscle contractions. It is more common in women under the age of 30 years and women who experience heavy periods.
Secondary dysmenorrhoea is pain that is caused by factors other than muscle contractions. It can be due to benign growths in the uterus such as fibroids. It can also be due to conditions such as endometriosis.
As highlighted above, period pain develops majorly due to muscle contractions in the uterus. These contractions are triggered by hormone-like substances called prostaglandins. Higher levels of prostaglandins are associated with more severe menstrual cramps. They can be caused by:
Endometriosis: A condition where the endometrial lining (lining of the uterus) grows outside the uterus, usually on the fallopian tubes, ovaries etc.
Uterine fibroids: Uterine fibroids are benign (non-cancerous) growths in the wall of the uterus
Adenomyosis: Adenomyosis is a painful condition where the uterine lining grows into the muscular wall of the uterus
Pelvic inflammatory disease: PID is an infection of one or more of the upper reproductive organs such as the uterus, ovaries or fallopian tubes. It can spread through sexual intercourse.
Cervical stenosis: Is a condition where the cervical opening is too small causing issues in regular menstrual flow. This results in a painful increase in pressure inside the uterus.
Painful periods can also be the result of several other underlying conditions. Your gynaecologist can help in identifying the root cause of the pain for a more effective treatment plan.
Also, read: Answers to Some Common Questions about Endometriosis
It is still unclear why some women have extremely painful periods while some experience no discomfort at all. Some of the risk factors of painful periods are:
If you experience extremely severe pain every month that impacts your daily life, your doctor can recommend any of the following treatment options:
This is the first line of defence against painful periods. Over the counter pain medications can be used to manage mild to moderate period pain. If required, your gynaecologist may also prescribe stronger pain killers.
In some cases, gynaecologists might recommend the use of hormonal birth control to prevent ovulation and reduce the severity of period pains. They should be used only if recommended. These medications also have several side effects, so make sure you are aware of them before you start taking them.
If your period pains are caused due to conditions such as endometriosis, your gynaecologist might recommend a surgery to treat the underlying condition. In some cases, hysterectomy (surgically removing the uterus) might also be done. However, this is the last resort.
If you believe that your pain is not severe enough to warrant a trip to the hospital, the following tips can help you relive some of the pain at home itself.
Apply a hot water bag or warm compress to your lower abdomen and back. You can even take a long hot water bath. This will help in relaxing your uterine muscles, giving you much needed relief from the pain.
While the dull ache in our muscles during our periods can make exercising tougher, physical activity is a proven solution for period cramps. Light exercise such as walking has been shown to reduce the intensity of period pains in some women. Yoga also has several exercises which are designed to relax the uterine muscles and reduce period pain.
Drink a lot of water and keep yourself hydrated during your periods for a smoother and less painful cycle.
While there is insufficient evidence to show the link between period cramps and diet, eating a balanced diet rich in vitamins and fibre such as lean meat, fresh fruit, green vegetables and whole grains, has shown to have a positive impact on our menstrual health.
Even today, there is a lot of stigma around menstruation and periods. There have also been several initiatives that started to address the problems caused by period pains such as corporates recognising “period leaves” every month. However, there is a long way to go in increasing awareness about menstrual cramps and pain. To know more about how to have a pain-free and smooth menstrual cycle, you can consult Dr Anjali Kumar at the CK Birla Hospital, Gurgaon.
Book an appointment with Dr Anjali Kumar.
Also, read: Lifestyle and diet tips for PMS
Growing up, we were taught many “rules” regarding how and what to eat. We were also told what habits to avoid while eating such as drinking water in the middle of a meal. While most of them are unfounded (ex: if you eat an orange seed you will grow an orange tree from your stomach), some of them are quite relevant (ex: don’t lie down right after a meal).
Whatever is said and done, stomach pains after a hearty meal are the worst! Especially for all the foodies out there. What’s more, pinpointing the exact cause of the stomach ache is quite challenging as the abdominal cavity houses so many organs. To make things a little simple, we have compiled a list of possible reasons for a stomach ache right after a meal.
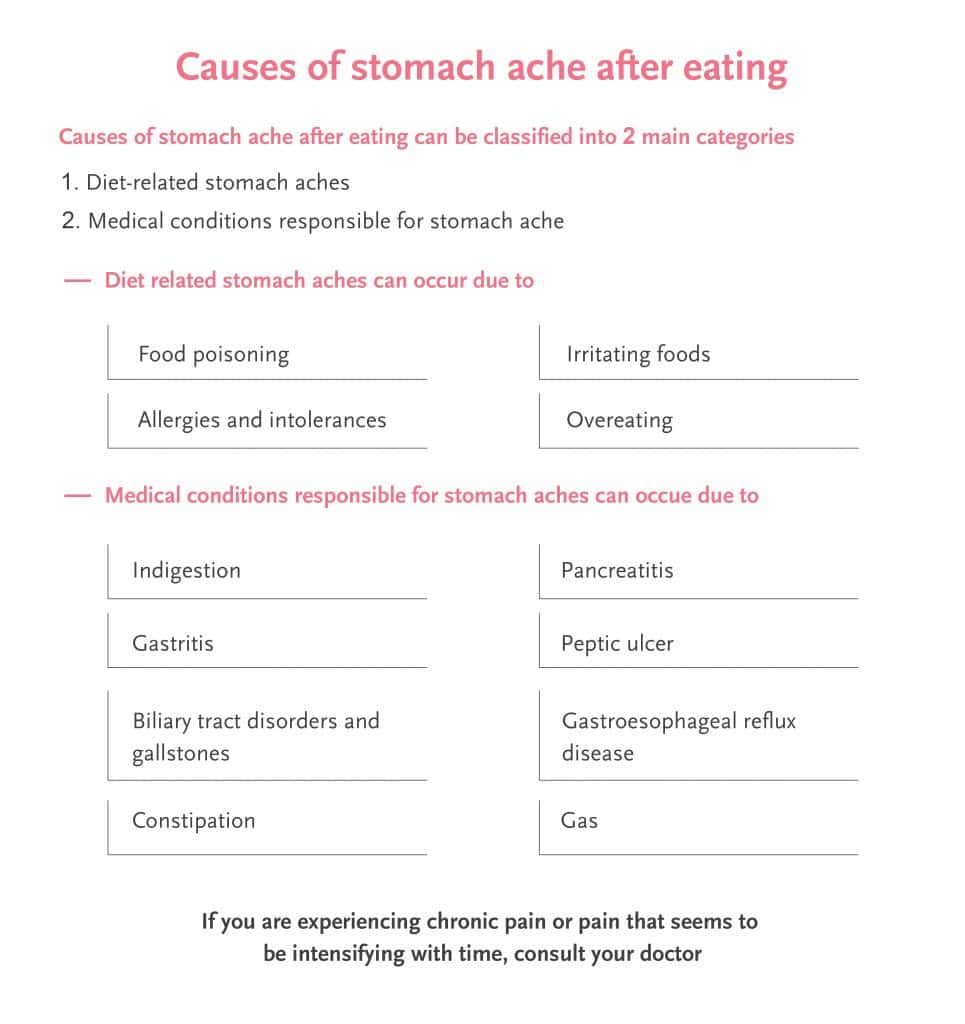
Table of Contents
We have all heard the saying “you are what you eat”. There is no doubt that whatever we consume has an extremely significant impact on how we feel. Here are a few reasons you might be feeling uneasy or queasy because of what you eat:
Sugary drinks and certain foods can cause bloating and wind. These include:
When someone chews gum, sucks sweets, or eats with their mouth open, it can lead to them swallowing air. This can be another cause of wind.
Some types of stomach pain need not be linked to “what” you eat. They can be caused by conditions that are triggered by “when” you eat. These include:
Read: Gallbladder Stones – Everything you need to know
If you are experiencing chronic pain or pain that seems to be intensifying with time, consult your doctor to seek the appropriate treatment. Many a time, the conditions can be managed by dietary and lifestyle choices provided they are diagnosed before they cause long term damage. If you are on any medications that seem to be causing stomach problems, consult your doctor for alternatives or supplements to manage symptoms.
Q1. Why do I get pain in my upper abdomen after eating?
Indigestion is one of the common reasons why one can get pain in the upper abdomen after eating. It gives a burning sensation in the upper abdomen and the sensation is carried to the food pipe and mouth as well. When there is too much acid or gas in the stomach the upper abdomen hurts.
Q2. What does pancreatitis pain feel like?
Pancreatitis pain is when an individual has pain in the upper abdomen which feels tender and sore on touching. This pan starts to radiate to the back.
Q3. Why do I get indigestion after I eat?
When the food is too palatable to stop even when the stomach is full that is when we start to overeat. Too much oily food, spicy food and too much sugar can result in indigestion.
A woman’s body undergoes countless changes throughout her life. From early adolescence to reproductive years and after, your body experiences a wide spectrum of changes. One such significant biological change – menopause – is part of this cycle of life. According to a study by the NCBI (National Center for Biotechnology Information), nearly 1.5 million women undergo the menopausal transition each year. However, only a few people understand what is menopause and how transitioning to menopause affects your body?
While it is neither a disease nor a disorder, transitioning to menopause can pose significant difficulties for most women. However, even today, there is a lack of candid and open discussions on menopause-related changes. Most women, therefore, cannot understand what they are going through or make sense of their feelings and emotions.
If you are a woman over the age of 45 years who is soon expecting her transition to menopause, then this article is for you. In the piece below, Dr Aruna Kalra, a leading gynaecologist at the CK Birla Hospital, talks about the different signs of menopause, what is menopause and what to expect from transitioning to menopause.
Table of Contents
Menopause refers to the natural decline in a woman’s reproductive hormones and the cessation of ovulation and menstruation. It is a biological milestone that is common in women between the ages of 45 and 55. The average menopause age in India is 46.2 years.
Menopause marks the end of the fertile phase of a woman’s life. Retrospectively, this is defined after 12 months or 1 year of amenorrhea (the absence of periods) has been observed. These changes, however, do not occur all at once.
Menopause occurs as a result of slowing down the reproductive cycle that has been continuously functioning since puberty. Due to the growing age, there are several levels of hormonal fluctuations that lead to a permanent stop at your periods.
If a woman loses her normal ovarian function before the age of 40, the condition is termed early menopause or premature menopause.
Menopause is characterised by hormonal changes and often involves troublesome symptoms such as vaginal dryness, vasomotor symptoms, insomnia, decreased libido, joint pain, and fatigue.
However, menopause body changes are not limited to these symptoms. Women may experience concurrent behavioural, psychological and social changes as well. Most of these symptoms are highly individual and may progress at a different pace for each woman.
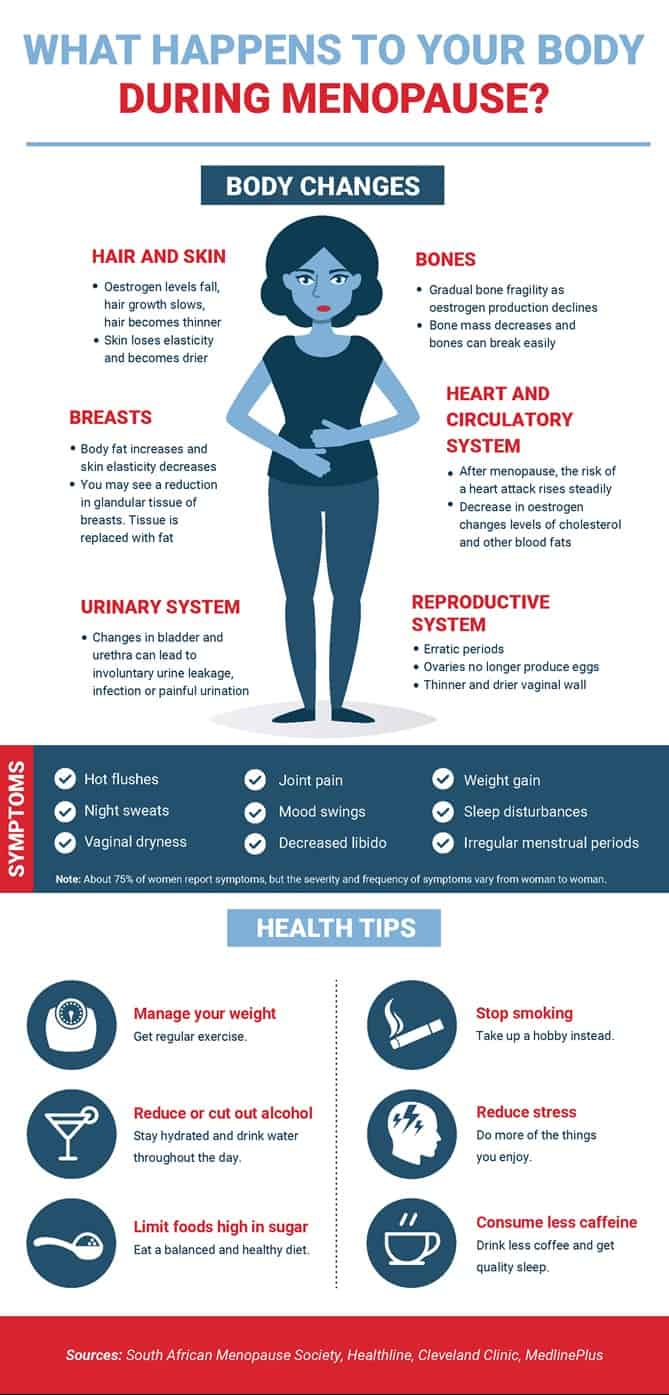
If you are at the cusp of the menopausal transition, here are 10 important body changes during menopause that you need to be aware of:
1) Hot flashes
Hot flashes are one of the most common signs of menopause and perimenopause. Hot flashes may last for a few or several years and are increasingly linked to low levels of estrogen.
Women who experience a hot flash (mostly the first sign of menopause) may suffer from sudden feelings of intense warmth, typically over the face, neck, and torso. They may also develop red blotches and break into heavy sweats.
2) Mood swings
Emotional upheavals and mood swings is another typical symptom related to menopause. Hormonal changes during menopause tend to experience rapid changes in mood due to a plunge in their levels of estrogen.
Estrogen can influence the interactions of serotonin and norepinephrine (feel-good hormones) on mood and cognition.
3) Anxiety and depression
Anxiety and depression are common but often overlooked symptoms of menopause. These feelings of irritability, anxiety, worry, and sadness tend to surface due to changing hormone levels.
4) Changes in the immune system
The immune system may become weakened due to body changes during menopause as a result of depleting hormone levels. As a result, women may become more susceptible to developing autoimmune diseases, allergies, and colds.
Menopausal women should try to boost their immunity by eating a nutrient-rich diet, managing stress levels, getting adequate sleep and consuming sufficient amounts of vitamins and minerals, especially vitamin C, zinc and vitamins A, D, and E.
5) Bone loss
An NCBI study documents that women lose about half their trabecular bone and 30% of their cortical bone throughout their lifetime. About half of this bone loss is said to occur during the initial 10 years after menopause.
Bone loss reportedly accelerates substantially during late perimenopause and early postmenopausal years. This rapid bone loss during menopause increases the risk of osteoporosis significantly.
Thus, menopausal women should eat foods that are rich in the following essential minerals and vitamins:
Apart from this, the DEXA (Dual Energy X-ray Absorptiometry) scan can also help determine if you have a low bone density or if you are at a high risk of experiencing fractures.
6) Low sex drive
Women naturally experience a lowered libido or sex drive as they go through menopause. This typically happens as a consequence of hormonal changes during menopause. Female hormones, namely estrogen and progesterone, decline during this period.
Symptoms such as vaginal tightness, pain during sex and vaginal dryness also frequently accompany the loss of libido or reduced sex drive.
7) Insomnia
According to the National Sleep Foundation, as much as 61% of menopausal women report symptoms of insomnia. Hormonal changes during menopause lead to changes in the natural circadian rhythm, causing disrupted sleep.
Other factors, such as a weak bladder, night sweats, joint pain, and anxiety, may contribute to insomnia as well. For this reason, women are frequently advised to do regular aerobic exercise and eliminate coffee, alcohol and other hot flush triggers before bed.
8) Ageing skin
Menopause can rapidly advance the ageing of the skin. A scientific study confirms this by pointing out that Type I and III skin collagen decreases by at least 30% in the first five years after menopause.
The body cannot keep up with the production of collagen because the estrogen levels in the body begin to decline.
9) Brain fog
Brain fog is another troublesome concern that many menopausal women face. Brain fog is characterised by forgetfulness and a lapse in focus or concentration. The brain has many estrogen receptors, so when it is robbed of this hormone, it cannot function as well as it used to.
10) Sudden weight gain
Weight gain is another common challenge that women experience during menopause. The inevitable loss of estrogen and progesterone can result in sudden weight gain.
Age-related factors such as – loss of lean muscles, increased stress, and sleep deprivation can also come into play.
Natural menopause is a gradual process that happens through three stages. The stages of menopause include:
If you are approaching the onset of a menopausal transition, the first thing you need to do is aware yourself of what is menopause and what are its possible effects on your body. You should prepare yourself for major physical and emotional changes.
If you experience severe menopausal symptoms, you can seek a variety of safe treatment options with the thoughtful use of estrogen or Hormone Replacement Therapy (HRT). For patients who are uncomfortable with hormonal therapies, there are alternative treatments as well.
To cope with symptoms of menopause such as night sweats, sleeplessness, and low sex drive, talk with our doctors at the CK Birla Hospital. Book an appointment with Dr Aruna Kalra, a leading gynaecologist in Gurgaon for personalised guidance during menopause.
Ques: What is the average menopause age in India?
Ans: The age of menopause in India is nearly 46.2 years.
Ques: How long do menopause symptoms last?
Ans: Menopause symptoms may last between 4.5- 7 years after the last period.
Ques: What are the most common body changes caused by menopause?
Ans: Common bodily changes of menopause include hot flashes, difficulty sleeping, memory problems, mood disturbances, vaginal dryness, and weight gain.
Ques: How many stages of menopause are there?
Ans: There are three stages of menopause – perimenopause, menopause and postmenopause.
Breast cancer is considered to be one of the most common cancers amongst women around the world. Even in India, the number of breast cancer cases reported every year is alarming, with breast cancer accounting for more than 27% of all new cancer cases. Every year, the month of October is celebrated as Breast Cancer Awareness Month as an effort to educate people about this devastating disease.
Dr Rohan Khandelwal, one of the best breast cancer surgeons in Gurgaon explains breast cancer in further detail to create awareness about the importance of routine screening and early warning signs to watch out for.
Table of Contents
Every part of our body is made up of different types of cells which multiply to replace old cells. In some cases, these cells can start multiplying uncontrollably causing a growth called a tumour. If these cells are normal cells, it is considered to be a benign tumour. However, if these cells are abnormal and do not function the way they are supposed to, they are considered to be malignant or cancer cells.
In the case of breast cancer, the cells of breast tissue start multiplying. In the initial stages, this is limited to the breast tissue. However, in advanced cases, it can invade and start growing on the tissue surrounding the breast. In more advanced stages, cancer spreads to the rest of the body, resulting in new tumours. This process is called metastasis.
While the exact causes of breast cancer are still unknown, several risk factors have been identified through years of medical research. It is still unclear why some women who have no risk factors can also develop breast cancer while some women who are at very high risk never get affected. It is best to stay cautious and aware of warning signs, risk factors and preventive measures.
A family history of breast cancer is a risk factor that should not be ignored. If any relatives in your family are affected by breast cancer, your risk of developing it is high. Today it is possible to do genetic testing to detect the presence of cancer genes. In such cases, preventative measures can be taken such as a mastectomy.
French fries, burgers, colas may be your favourite snacking options, but do not ignore the damage they cause. Red meat, saturated fats, processed food can all cause cancer of the breast, stomach, bowels, mouth and food pipe. It is important to follow a balanced diet with plenty of fibre-rich food, whole grains, fruits, vegetables etc. Switch to lean proteins such as chicken and fish. Consuming a little bit of turmeric daily has also been shown to have positive benefits.
Obesity is a complex condition that can result in several health complications such as heart disease, hypertension, type II diabetes etc. Being obese or overweight can also increase your chance of getting breast cancer, especially if you are post-menopause. In such cases, you are advised to go for breast cancer screening with a mammogram at least once a year. Breast cancer is easily treated if detected early. Hence, routine screening goes a long way in minimising the impact of breast cancer.
Regular consumption of alcohol increases your risk of developing breast cancer.
Consumption of tobacco especially smoking, can result in a wide range of illnesses including cancers of the head and neck as well as breast cancer. There are several support groups available to help people quit smoking.
Related Read: Everything you need to know about breast density
Unfortunately, there are still no ways to completely eliminate the risk of breast cancer. Risk factors such as inherited changes in certain genes (BRCA1 and BRCA2), family history etc are beyond our control. You can however minimise its impact by detecting it early on. Early detection offers the best protection against breast cancer.
In your busy life, how often have you looked and felt your breasts to spot any changes in them? Every month, performing a breast self-examination is recommended. This will help you familiarize yourself with your breasts, enabling you to detect any changes easily.
Ideally, you should consult a doctor if you spot any change in your breast. This can range from an unusual pain that doesn’t go away or any type of discharge.
The following signs are indicative of changes in your breast and possible symptoms of breast cancer that need immediate attention.
Read: Breast Cancer Symptoms and Warning Signs
Keep checking for any abnormalities/unusual changes in your breast from time to time. It is recommended that if you are over 40 years of age, you should seek annual breast cancer screening with a mammogram. Breast cancer in the early stages may not even require surgery. Hence early detection is your best chance against breast cancer. Consult our experts/surgeons at The Breast Centre to assess your risk and help detect breast cancer in its early stages.
Most certainly, you would have experienced the distress of a headache, sometime in your life. Remember the throbbing, sharp pain that disrupts your routine and does not seem to get any better? Now double the intensity and time of that pain and what you get is a headache disorder called migraine. Migraine headache affects nearly 1 billion people across the globe. It is a condition characterized by repetitive debilitating headaches, scaling from moderate to severe. According to the Migraine Research Foundation, migraine headache is the third most common illness in the world. Despite such high incidence, there is little understanding of migraine symptoms, causes and treatment.
In this article, Dr Tushar Tayal, a leading internal medicine specialist, explores what is a migraine and what are the migraine symptoms?
Table of Contents
Migraine is a very common disorder. It is a neurological condition that causes extreme pain and a pulsing sensation at one side of the head may last for several hours and may extend up to days.
A migraine is more than just a headache as it generally follows after an aura of sensory disturbances. These aura disturbances include:
The pain is known to worsen if the patient is involved in any type of physical exertion. Migraine tends to affect people aged between 15 to 55 years.
Migraine meaning can be classified into two main types which depend on whether the patient suffers from sensory impairment or disturbances. These disturbances are known as aura. Hence, the types of migraine include:
These symptoms act as warnings for many patients and signal the onsets of migraines. An aura is characterised by various sensory disturbances which include:
As the name suggests, under this category, a patient does not feel any aura impairments or sensations. Nearly 70% to 90% of people experience migraines without any sensory disturbance or aura.
However, even in migraines without aura, a person undergoes the onset or the beginning of the migraine attack and experience symptoms one or two days before. This state is known as the prodrome stage.
Besides a classification based on aura, types of migraines are further divided. There are a few other types of migraine that are related to specific syndrome and triggers.
While it is important to learn about the symptoms, you should not self-diagnose your condition. It is highly recommended to see a doctor if the headaches follow a migraine pattern.
Migraine symptoms vary from their type and stage of the onset of the headache.
The common migraine symptoms in the prodrome stage include:
In migraine with aura, some sensory difficulties are experienced by the patient after the prodrome stage. During Aura sensory organs are affected with impairment in vision, movement, hearing, speech and/ or sensation. Common migraine headache symptoms with aura include:
The notorious migraine pain occurs afterwards. This stage is called the Attack phase. The most severe of all phases for which migraine is known. This phase can last up to hours or even days. Symptoms seen in this phase can vary from person to person. Some of the most common migraine symptoms of the attack phase include:
After the attack, the patient generally experiences what is called the postdrome phase. Changes in mood and feelings are experienced during this phase. This can range from elated and happy to fatigued and apathetic with a mild and dull headache.
The duration and degree of these phases vary from person to person. It is not unusual for a phase to skip and it is completely possible that an attack may occur without any headache.
The migraine causes are not fully understood yet. But apparently, the cause is a mix of genetics and environmental factors that play a major role and can be considered reasons for migraine.
Abnormal brain activities may result in migraine pain. This affects the way nerves communicate and may cause a chemical imbalance. This imbalance includes a decrease in brain chemical known as serotonin. Genetics and allergies also seem to play a big role. In the above two-third of the cases, migraine runs through the family.
A migraine trigger is any environmental change, external stimulus or physical act that results in a migraine headache. Many triggers are responsible and reasons for migraine attack which includes:
There is no single cure for migraines and the treatment may vary from person to person. It is highly recommended to see a doctor if you see any of the symptoms mentioned above or if your headache follows a migraine pattern.
Migraine treatment helps in preventing a full-blown attack. Sometimes migraine may alleviate merely with some changes in lifestyle and daily habits but sometimes it may need surgery to cure. The best way to deal with migraine is to consult a doctor and get it diagnosed.
Medical treatment and lifestyle modifications, combined can help in getting rid of a migraine. Some lifestyle changes may help with a migraine which includes:
Generally, migraine medication is also advised as a course of treatment. Always consult a doctor before starting any kind of migraine medication.
The primary difference is the fact that migraine is a headache disorder. It is one of the many types of headache. Generally, a headache is felt in the head, face or upper neck area. While migraine headache is felt mostly at one side of the head.
A migraine headache can be a draining experience and consume several hours or even days of your life. It is important to educate yourself about the fundamentals of migraine to seek effective migraine treatment.
For more information or personalised guidance, book an appointment with a leading internal medicine specialist or call us at +91 124 4882248.
Ques: Can migraine go away on its own?
Ans: Yes, it is possible that a migraine headache may subside on its own. However, if your headache is severely affecting your daily life, you must seek clinical help.
Ques: How can I get rid of a migraine fast?
Ans: You can apply a cold or hot compress on your head, dim the lights around you and drink plenty of water to help get rid of a migraine.
Ques: Which foods can relieve migraine?
Ans: Some well-known foods that can help relieve migraine include sweet potatoes, carrots, spinach, brown rice, and more.
Ques: What should be avoided during a migraine?
Ans: You should identify and avoid your migraine triggers such as aged cheeses, alcohol and caffeine.
Kidney disease is one of the most underestimated illnesses that affect people across age groups. Nearly 14% of the total general population lives with chronic kidney disease (CKD). According to the National Kidney Foundation, CKD is accountable for more deaths than breast or prostate cancer. Despite such high incidence, there is a substantial lack of awareness about kidney disease symptoms.
In the article below, Dr Mohit Khirbat, a renowned nephrologist in Gurgaon, discusses the various signs of kidney disease that one must be aware of.
Table of Contents
Before we set on to discuss the common signs of kidney disease, it is important that we understand what kidney disease means?
As the name suggests, kidney disease is an ailment of the kidneys. Your kidneys are two bean-shaped organs located at the back of the abdomen right below your ribcage. Kidneys are responsible for the following functions –
Having kidney disease means that your kidneys are unable to perform the above-given functions properly. Kidney disease has various complications – a damaged kidney can affect the process of filtration in your body. As a result, waste and toxins can collect inside your body leading to health problems such as nausea, weakness, poor sleep, and shortness of breath.
Kidney disease is generally classified into two categories, based on their causes – acute kidney disease and chronic kidney disease.
As mentioned above, chronic kidney disease develops over several months or even years. This ailment often shows several early signs of kidney disease.
Here are some common symptoms of kidney disease you should know:
1. You are more tired: Fatigue is among the first early signs of kidney disease. In a small cross-sectional study of nearly 87 patients living with advanced chronic kidney disease, profound fatigue was noted as one of the top symptoms of kidney disease.
When your kidneys stop working with their everyday capacity, you tend to develop a buildup of toxins and waste in your body. These impurities can make you feel easily tired.
In addition, you may also see a significant drop in your energy levels. The collection of these toxins can also contribute to a decreased level of concentration. International Society of Nephrology (ISN) notes that fatigue is also a sign of depression which is commonly seen in patients with advanced renal disease.
2. You have difficulty in sleeping: There is a well-established link between sleep and kidney function. Your sleeping pattern impacts your kidney’s health and its functions.
According to the National Kidney Foundation, your kidney function is regulated by the sleep-wake cycle. Your kidneys function 24 hours a day and your sleep cycle helps in coordinating its workload. Patients living with chronic kidney disease experience a variety of sleep disorders.
A poor sleep pattern, increased sleepiness during the day, poor nighttime sleep and more among the early signs of kidney disease. The primary reason for these signs is the collection of toxins in your body.
3. You have an increased need to urinate: Damage to the filters of your kidney can lead to increased urination, especially during the night. Having an increased urge to urinate at the night (nocturia) is a well-known sign of kidney disease.
Nocturia is remarkably common in chronic kidney disease with approximately 64 % affected patients.
4. You see blood in the urine: When you think about what are the signs of kidney disease, you must consider the presence of blood in the urine. Your kidneys are responsible for filtering toxins from your blood. In this process, they usually reserve the blood cells.
However, when the kidney function is damaged, some of the blood cells begin to leak and appear in the urine.
5. You have swollen feet and ankles: Another vital function of your kidneys is to balance the levels of fluids in your body. When you are living with kidney disease, the excess fluid cannot escape and gets collected in your body. This accumulation of excess body fluids can lead to swelling in your feet and ankles.
6. You experience a loss of appetite: Due to kidney damage, you are likely to experience a variety of toxins remain in your body. This pile of toxins can affect your eating habits and appetite.
Several people (nearly 10% of people experiencing end-stage renal disease) experience a loss of appetite as one of the early signs.
7. You have skin dryness & itching: Other signs and symptoms of kidney disease include skin dryness and itching. Dermatological issues pertaining to the skin are highly common in people living with chronic kidney disease or end-stage renal disease with almost 40% of the patients being affected.
Skin itching may vary from moderate to severe in person to person. Dry and itchy skin is also a sign associated with mineral and bone disease, that is often found in people living with kidney disease.
8. You have foamy urine: One of the most common kidney disease symptoms includes having foamy urine. When your kidney gets damaged, it allows for a large amount of protein to leak out through urine. This protein presents in the form of foamy urine – with bubbles.
9. You feel muscle cramping: One of the common kidney disease pain symptoms is muscle cramps or twitches. As a result of reduced kidney function, your body is not able to regulate fluids and electrolytes leading to cramping. Components such as reduced calcium or phosphorus levels are leading factors for this symptom.
10. Your eyes are puffy: When your kidneys are not working properly, various minerals and protein get collected in your body. The accumulation of these components may settle be displayed in the form of puffiness under the eyes.
Additionally, chronic kidney disease is caused by diabetes and high blood pressure which can put a strain on the blood vessels of your eyes leading to vision problems.
Your ideal method of treatment for kidney disease will depend upon its cause, the severity of your symptoms, stage of kidney disease and your overall health.
Majorly, there are four treatment options available to patients living with kidney disease:
You can expect to feel kidney pain on your sides or middle and upper back areas. Sometimes, the pain experienced due to kidney disease can also progress to the abdomen or groin.
If you are wondering – is back pain a symptom of kidney disease? – the answer may be, yes. However, kidney pain in the back can also be caused due to other health conditions. It is best to consult a verified nephrologist in case you experience this symptom.
Kidney disease symptoms can be easily misinterpreted. It is essential for people of all ages to understand these signs and symptoms so that you can practice prevention and take the necessary treatment at the right time.
For more information, book an appointment with Dr Mohit Khirbat, a leading nephrologist at the CK Birla Hospital.
Ques: What is the first sign of kidney disease?
Ans: Fatigue, loss of appetite, foamy urine and changes in urinary output are some early signs of kidney disease.
Ques: What are the stages of chronic kidney disease?
Ans: Chronic kidney disease progresses over time through five stages. These are:
Ques: How can I protect my kidneys?
Ans: You should restrict your sodium intake, limit caffeine, exercise regularly and get plenty of sleep to protect your kidneys.
Ques: Which are the best foods to protect kidney function?
Ans: Top foods for better kidney function include cauliflower, blueberries, egg whites, garlic, cabbage, olive oil, bell pepper and onions.
Irritable and itchy anal cavity, trouble passing stools, bloody stools, and discomfort when you sit for a long time? – chances are you may have experienced these conditions at some point in time in your life. You’re not alone! 50% of the Indian population suffers from haemorrhoids. It is reported that 20% of cases suffer from piles and fissures together. However, many of us often fail to understand the fundamental difference between piles and fissure since both have similar symptoms.
In this article, Dr Mayank Madan, a leading general surgeon in Gurgaon, explains the difference between piles and fissures.
Table of Contents
Piles or haemorrhoids are inflamed veins in the rectal or anal region that may protrude outside, causing discomfort.
An anal fissure, on the other hand, is a small cut on the lining of the anal cavity.
Here are some essential differences that can help you understand what are piles and fissures.
| Piles | Fissures |
| Swollen veins in the anal canal, rectum or anus | Tear or cut of anal skin |
| Painless during the initial phase and increases as the swelling becomes more prominent | Very painful and uncomfortable with little or more bleeding |
| Piles are a result of prolonged constipation, pregnancy or chronic cough, physical strain | This occurs during pregnancy, as a result of obesity or an injury to the anal cavity, to people with Crohn’s disease, passing hard stools and chronic diarrhoea |
Piles Vs fissures are often misinterpreted due to overlapping signs and symptoms. Here is a detailed overview of piles fissures to help you grasp a better understanding.
Piles can be broadly categorised into three types:
The symptoms and treatment options purely depend on the kind of haemorrhoid you have and its severity. When deduced in the initial stages, you can even treat it with simple lifestyle changes and natural home remedies.
Internal haemorrhoids occur as hard lumps in the back passage inside the rectal cavity. You might not feel them initially as that region has very few pain-sensing nerves. However, in case you have prolonged constipation or strained bowel movement, then this can cause occasional bleeding and pain.
Internal haemorrhoids can be further classified based on their severity:
Some of the standard inner piles’ symptoms include:
External haemorrhoids are more prominent and painful as they occur in the outer region of your anal canal. They usually are covered with regular skin and have pain nerves surrounding them. This variant of piles is more painful and has a high risk of clots, skin tags, and other related skin infections.
Thrombosed haemorrhoids are characterised by a blood clot that prevents blood flow. Sometimes these haemorrhoids burst and start bleeding due to excessive blood. If you are wondering if these are bleeding haemorrhoids are dangerous, worry not! Although thrombosed haemorrhoids can cause a lot of pain and discomfort, they are usually benign.
Unlike piles, anal fissures can be very painful right from the beginning. The light tear on the moist tissue of the anal region can cause painful itching and spams in the anal sphincter.
Depending on the severity of the condition, fissures can be categorised as:
Acute fissures are freshly developed and thus, can be treated easily. One can encourage the self-healing of these fissures with simple home remedies.
If left untreated, however, they can manifest as chronic fissures in the future.
These are fissures that last for more than 8-12 weeks and need medical assistance to heal.
Along with the anal tear, chronic fissures also involve a swelling commonly known as a skin tag, and extra tissue growth known as hypertrophied papilla.
Usually, anal fissures entail a searing pain at the bottom. However, other fissure symptoms that you may experience are:
A typical fissure or haemorrhoid is easy to manage and would take a minimum of 6-8 weeks to heal completely.
You can try the following methods for the best treatment for piles and fissure for faster healing:
Depending on the severity of the condition, your medical practitioner might prescribe stool softeners, over-the-counter creams and topical ointments.
One can treat these health issues without operations, but in severe cases, your doctor may suggest surgery of piles and fissure. Depending on your condition, you can also opt for advanced methods including laser treatment for piles and fissure.
Certainly, you would know the difference between fissure vs piles. However, their symptoms can be managed by slightly altering your lifestyle.
Here are some recommendations you should follow if you are suffering from piles and fissure:
You can prevent the onset of piles fissures with good lifestyle choices. The preventive measures for these conditions entail promoting healthy bowel movement.
For many people, discussing anorectal disorders can be embarrassing and acts as a barrier to getting the right care. But these issues are liable to worsen if not addressed immediately. To seek the right care, it is essential to stay informed about your condition. Thereby, one should know the primary difference between piles and fissure. To avoid further health complications, one must seek medical advice as early as possible.
To get the best laser treatment for piles and fissures, visit CK Birla Hospital or book an appointment a leading general surgeon in Gurgaon.
Ques: What is the primary difference between piles and fissures?
Ans: Piles are swollen blood vessels while fissures are cuts, tears or cracks of the anal skin.
Ques: How to get rid of piles permanently?
Ans: To get rid of piles permanently, you should eat high-fibre foods, more fruits, vegetables and whole grains.
Ques: Can piles and fissures occur together?
Ans: Piles and fissures can happen together or separately.
Ask a pregnant woman how she is feeling and you will hear either absolute happiness or absolute discomfort. During the route of pregnancy, there seems to be no in-between. While pregnancy is a beautiful phase, it comes with its own share of distress, for instance – back pain. Approximately 50-80% of women are affected by lower back pain pregnancy. However, there is a very simple solution to this worry – physiotherapy during pregnancy.
Physiotherapy in pregnancy is an effective practice to reduce painful symptoms such as lower back pain, pelvic pain and involuntary urination.
In this article, Dr Aruna Kalra, a renowned obstetrician & gynaecologist at the CK Birla Hospital explains the various benefits of physiotherapy for pregnant women.
Table of Contents
Physiotherapy, also known as physical therapy, is an evidence-based technique that involves the science of movement to promote healing and holistic fitness. It includes a wide array of exercises and massages.
While any person, irrespective of age and gender, can benefit from this technique, physiotherapy during pregnancy has well-defined advantages.
Our body produces a hormone known as relaxin. While both men and women form relaxin, this hormone is primarily produced in pregnant women. It is responsible for preventing any damage to a woman’s body during childbirth.
The production of relaxin increases significantly during the second trimester. Primarily, this hormone is aimed at the loosening of the birth canal and preparing your body for childbirth. However, besides the birth canal, high levels of relaxin result in the loosening of other ligaments in your body. While on one hand relaxin facilitates the flow of blood, it leads to muscle, joint and body pain, on the other. This side-effect of relaxin is the fundamental cause of your lower back pain pregnancy. The transitory loosening during this period of pregnancy can make your muscles and ligaments weak for a long period of time.
Physiotherapy during pregnancy is a helpful approach in dealing with the pain resulting from an increase in relaxin. This practice can assist in alleviating from muscle pain through the means of specific exercises and massages. The targeted exercises not only help in reducing pain but also maintain the strength of muscles.
As discussed above, antenatal physiotherapy can help in reducing pain and improving the strength of muscles. While a majority of pregnant women complain of the lower back pain, there are other areas that physical therapy can help with.
Some common issues pregnancy physiotherapy can deal with are:
It is important to remember that the source of your pain and discomfort is the increase in levels of relaxin. However, the location of your pain can be unique. The role of physiotherapy in pregnancy is identifying the precise location of the pain and addressing it to minimise ache.
Physiotherapy benefits pregnant women in multiple ways. The role of physiotherapy in pregnancy has both, long and short-term advantages. Some of the top benefits include:
As your pregnancy progress across three trimesters, physiotherapy and exercise during pregnancy also vary.
1. First trimester: The first trimester is the time when you are just getting used to pregnancy and the various changes it brings. Your physical activity, diet and physiotherapy will aim at assisting you in getting used to these changes. Your physiotherapist will begin by educating you and your partner about maternal and fetal changes and what to expect.
Physiotherapy in the first three months focuses on your posture, challenges at home and work and pre-existing musculoskeletal problems (if any).
Your physiotherapist will slowly assist you in correcting your postural at workplace and home. He/she will offer you techniques for safe lifting and mobility and treat any musculoskeletal problems you had been suffering from.
2. Second trimester: By the second trimester, you are well into pregnancy and accommodating the tremendous changes in your hormones and your body. Physiotherapy in the second trimester of pregnancy helps you in keeping up with these shifts.
Your physiotherapist will start exercises after completion of the anomaly scan and with clearance from your primary consultant.
Physiotherapy in the second trimester focuses on stretching techniques to improve the flexibility of the lower limbs and pelvis. You will be instructed to do mobility and strengthening exercises for the spine and the abdomen. The goal of this exercise during pregnancy is to enhance fitness and emphasise on pain management.
3. Third trimester: By the last three months of your pregnancy, your physiotherapist will focus on promoting strength and flexibility. You will be assisted towards labour coping strategies such as relaxation techniques, breathing exercises, positioning to facilitate labour and techniques to use in the pushing stage.
Physiotherapy in the third trimester of pregnancy involves advanced strengthening for the spine and abdomen, pelvic floor exercises, techniques to improve the flexibility of the lower limbs and pelvis and pain management.
Your choices during pregnancy will help in deciding the health of your fetus. Physiotherapy during pregnancy is a preferable choice for expectant women who wish to inculcate exercise and relaxation in their life.
Make sure to visit a verified and qualified physiotherapist and follow their correct instructions to avoid any complications.
For personalised guidance on antenatal care, book an appointment with Dr Aruna Kalra, the best obstetrician in Gurgaon at the CK Birla Hospital.
Is physiotherapy safe during pregnancy?
Yes, physiotherapy is a completely safe and effective method of pain management, exercises and relaxation during pregnancy.
How can physiotherapy help in pregnancy?
Physiotherapy during pregnancy has a large number of benefits. It helps an expectant mother to engage in physical activity, relaxes sore muscles, strengthens muscles, improves flexibility and offers pain management.
Is exercise recommended during pregnancy?
Yes, nearly 30-40 minutes of regular exercise is recommended for pregnant women to have a smooth and safe pregnancy, labour and childbirth.
Who should not exercise during pregnancy?
A pregnant woman who is suffering from severe anaemia, chronic heart or lung conditions, placenta previa or other complications should avoid doing exercise.
Congratulations on becoming a new mother!
A brand-new era of your life is about to start. Needless to say, with a baby in your life, your routine must have turned upside down. However, the birth of a child does not only affect your routine but also your bodily functions. After delivery, your body tries to get back to how it was before pregnancy. Externally, you will notice a change in your size and shape. Internally, your organs will resume their functions to maintain your health, meaning, you can also expect your periods after delivery.
In this article, Dr Anjali Kumar, a leading obstetrician at the CK Birla Hospital, Gurgaon, discusses all that you should know about your first period after delivery.
Table of Contents
During the 9 months of your gestation, there is a break in the process of menstruation. It is a matter of simple biology that while you are hosting a fetus in your womb, you will not have periods. For most women, this gap is welcomed with a sense of relief. Thanks to pregnancy – you don’t have to worry about staining your trousers or deal with premenstrual syndrome for several months.
Nonetheless, periods after delivery make a comeback and it is, often, unpleasant. You should aware of first menstruation after pregnancy in advance to avoid any additional discomfort.
Your first period after pregnancy will not come almost instantly. The time period of menstruation post-delivery for every woman is varying. If you are wondering, after delivery when periods will come? The answer lies in the practice of breastfeeding.
If you are not breastfeeding your newborn, you can expect your cycle to start in 6-8 weeks. This time can also vary from one woman to another. On the other hand, if you are exclusively breastfeeding (meaning that your child is only feeding on your breastmilk), your periods can delay even more.
The link between varying times of breastfeeding and periods exists entirely because of hormonal function. Prolactin hormone that helps in the production of breast milk can suppress reproductive hormones. Due to this suppression, your body is unable to ovulate and menstruation is halted.
Getting your period will also affect your breastmilk to some extent. The overlap in hormones affects your breastmilk which can be felt by, both, you and your child. Your period may affect the composition or taste of your milk or there may be a decrease in supply. Every woman experiences some type of change differently. However, as these transitions are temporary, they should not be a cause of concern for the mother.
The long lag in the resumption of the menstrual cycle can make you wonder – does menstruation occur after pregnancy? But yes, it does. There is no well-defined schedule for when menstruation will happen. However, if you have any concerns or worries, you should address them to your obstetrician.
First postpartum periods appear for everyone differently. It is evident that your body has been tremendous changes through the course of pregnancy and would require time to readjust. Coming back to normalcy will be a gradual process. Until then, the natural biological processes will affect your body somewhat uniquely.
Since your body is again adjusting to the process of menstruation after a lengthy gap, you can expect some changes. Some top changes include:
The majority of differences in your periods after pregnancy is due to the extra collection of uterine lining that needs to shed. Due to this extra lining, you are likely to experience intense pain and cramping. With time, these symptoms will reduce and your body will get back to normal.
A variety of health concerns prior to pregnancy can affect your postpartum periods. For instance, if you were suffering from thyroid, you are likely to experience a heavier flow.On the other hand, if you were suffering endometriosis before pregnancy, your first period after pregnancy may be lighter.
Your postpartum periods after cesarean delivery are not majorly different from periods after a normal vaginal delivery. You can expect vaginal discharge and heavier bleeding because your body is trying to shed the tissues that were lining your uterus during pregnancy.
Initially, during postpartum, you can expect to notice heavier flow and clots in your periods. Over time, your flow will become light and provide a way to a creamy white or red colured discharge called lochia. This vaginal discharge, lochia, continues for upto 6 weeks by which time you will get your first period.
Lochia is a great indicator to identify postpartum period symptoms. You can identify whether you bleeding is associated to periods or if it is related to some other health complication. Lochia has a very distinct odour which cannot be identified as foul. It become lighter in colour and texture, gradually. Pregnancy-related discharge increases with exertion or activity.
If your postpartum period symptoms do not match the above given description, you should consult your healthcare provider for a checkup.
An ectopic pregnancy is one in which the fertilised egg implants itself outside the uterus. Ectopic pregnancies are uncommon and may require extensive recovery.
Periods after ectopic pregnancy may occur anywhere between 2-10 weeks. You can expect your first period after ectopic pregnancy to be more painful. However, the symptoms are usually manageable.
It is evident that your periods after pregnancy are going to be heavier and painful. However, these symptoms should not aggravate to a level of unbearable discomfort.
Watch out for the following symptoms:
Apart from these symptoms, if your periods have been absent for more than three months after you have stopped breastfeeding or if you notice that your menstruation is relatively scarce, you should talk to your doctor immediately.
Most women return to their normal cycle soon after giving birth. If your period was ‘normal’ prior to pregnancy, it will occur every 21 to 35 days post pregnancy, while the bleeding may last anywhere between 2 to 7 days.
However, ‘normal’ here may also relate to what you were experiencing before your pregnancy. If you have a history of painful periods or endometriosis, for example, you will likely continue to have painful periods over time.
In the weeks after birth, your body is still as fragile as it was during pregnancy. While you may be eager to return to your regular routine quickly, you must take things slow.
Avoid heavy lifting or doing any strenuous exercise. Most importantly, follow all your doctor’s instructions for recovery and ensure that you go for your postnatal checkups regularly. A comprehensive postpartum checkup should be done within 4 to 6 weeks after giving birth.
By learning about periods after delivery or postpartum health, you can prepare in advance and cope with the symptoms in a better way.
For more information, consult Dr Anjali Kumar, a leading obstetericin and gynaecologist at the CK Birla Hospital.
Do periods start immediately after delivery?
You can expect your periods to start within 6 weeks of delivery. However, the time may vary since every woman is different.
Can I get pregnant after delivery without period?
Yes, you can get pregnant again before getting your first period after previous pregnancy if you ovulate timely. However, you will not be fertile immediately after delivery.
Do periods hurt more after C section?
You are likely to experience heavy and painful periods irrespective of normal delivery or C-section.
Will my period affect my breast milk?
Yes, you may expect a decrease in breastmilk supply when you get your first period post pregnancy.