Filter :
When planning and undergoing pregnancy, nobody is more excited than the expectant parents, for the baby’s arrival. Counting days is normal in this state of euphoria. But it’s not just you but also your doctor who has to count the days to understand how the little blip in your womb is growing and developing before it arrives healthy and happy.
This concept of counting days in medical terms is called a gestation period. It is a vital part of your pregnancy, not just for you but also for your OB-GYN. So let us understand what is the significance of a gestational age as we read ahead.
Table of Contents
The time period between conception and childbirth is called the Gestation period. This is the period during which the baby develops inside its mother’s womb. Therefore, gestational age is commonly used to describe how far along the pregnancy is at that given point in time. Usually, it is measured in weeks.
Pregnancy has to be carefully monitored to help keep it smooth and free from complications. This is why the gestational age becomes a vital piece of information needed by doctors. It helps them identify the right time to perform various tests and assessments of the baby and the mother’s health at different points throughout the pregnancy.
The thumb rule is: we start from the first day of the expectant mother’s last menstrual cycle to the date on which we are currently prior to the delivery. The gestational age ends with childbirth, however, it can be determined before or after birth.
A normal pregnancy tenure lasts between 38 to 42 weeks. This is why gestational age is also measured in weeks. A child born before the completion of 37 weeks, is considered premature. And if they are born after the 42nd week, they are considered postmature.
Gestational age before birth can be ascertained through ultrasound imaging, where your healthcare partner will measure the baby’s size, especially that of its head, abdomen, and thigh bone. This gives a clear indication of the baby’s fetal development in the womb.
Gestational age can be measured after birth by physically examining the newborn’s weight, length, head circumference, vitals, reflexes, posture, muscle, skin and hair. When the baby’s gestational age equals its calendar age, then the baby is said to be Appropriate for Gestational Age (AGA). These children have lower mortality rates than those who are born too small (SGA) or large (LGA) for their gestational age.
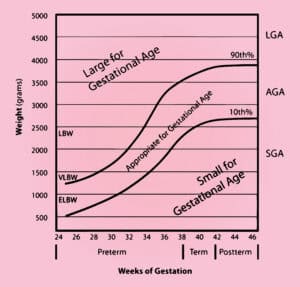
Source: Gestational age chart, how to calculate gestational age & corrected age (healthjade.net)
Over the years ultrasound has emerged as an accurate method of assessing gestational age, especially through transvaginal and transabdominal probe assessments. Transvaginal USG is preferred during the first trimester of pregnancy. Here are some of the sonographic methods of evaluating gestational age:
USG within the first 13 weeks and 6 days gives the best estimate of gestational age. Here, the transvaginal approach often provides a more clear and more accurate view. The gestational sac and yolk sac are the first visible markers, but sometimes they don’t really correlate with gestational age.
If it is not determined within the first trimester, then the crown-to-rump measurement of the foetus is considered a good way to assess the development during the second trimester as the baby is bigger and more palpable to USG imaging.
This is an old but proven method where postnatal gestational age is determined on a point-scoring pattern based on physical and neurologic assessments of tone, patterns, reflexes, movements, abnormalities, and behaviours. Higher scores translate to greater maturity.
This is an improved postnatal scoring system used for premature babies. It assesses 6 physical maturity components: skin, lanugo, plantar creases, breast, ear/eye, and genitals. And six neuromuscular components: posture, wrist, arm recoil, heel to ear, etc.
However, there are other non-sonographic methods also used to measure gestational age.
Identifying the gestational age accurately is the task of fertility experts and gynaecologists. The team of experts at the CK Birla Hospital, Mother and Child Department will not only help you plan your pregnancy smoothly but will also regularly assess your and your baby’s health and development to promptly identify any complications that can be completely averted.
Miscarriage is most likely to occur during the first trimester of the pregnancy itself. The commonly noted gestational age is around 12 weeks. However, it must be noted that the first trimester is the time when most miscarriages take place without the person knowing they are pregnant. Due to a hostile environment in the womb, the fertilised egg does not develop and the body miscarries the pregnancy.
When a pregnancy terminates before 24 weeks, it is termed a miscarriage. Miscarriages are common in the first trimester due to developmental problems with the baby in the womb. It can happen early on in the pregnancy, even before 14 weeks.
A full-term pregnancy lasts for 9 months. To assess the bodily changes and foetal development, these nine months have been divided into 3 equal parts of three months each. This is why they are called trimesters. However gestational age is measured in weeks, so it is not the same as a trimester. But if the pregnancy has completed 13 weeks of gestation, it has completed a trimester. Trimesters apply to the pregnant mother, gestational age applies to the growing baby.
Gestational age is measured from the first day of your LMP or last menstrual period. Fetal age is calculated from the actual date of conception, that is when the woman is ovulating. This implies that the fetal age is approximately two weeks behind the gestational age, which is the actual age of the fetus.
Pregnancy is a wonderful time when a woman is filled with the hopes of giving birth to a whole new life and preparing for the sleepless nights that lie ahead. By sleepless nights we not only mean the nights after birth, handling the newborn, but the nights full of anticipation towards the time ahead. Usually, as the baby grows inside the womb, the mother also grows in size. The pregnant belly makes it very difficult to sleep sometimes. As the delivery date nears, sleeping postures keep changing to accommodate the baby and keep the mother calm and at ease.
However, did you know that sleeping postures can sometimes create unnecessary complications in your pregnancy? That’s right. Pregnant women need to be mindful of how they sleep in order to avoid complications at birth. To know which postures are ideal and what are the necessary precautions for the mother and her baby, read on…
Table of Contents
When you’re pregnant, getting a peaceful and uninterrupted sleep can be hard. As your body grows to accommodate the growing baby, it gradually becomes tougher to find a comfortable sleeping position. The main causes of interrupted sleep are:
In conclusion, sleeping is essential for the baby’s growth and it keeps the body of the mother well rested. Not getting sleep or restricted sleep is very common during these delicate times. Therefore, it is advisable to ensure that you are monitored throughout, with a hands-on healthcare partner, who is available to advise patients on how to keep their pregnancy going smoothly. If you seek advice, then we recommend you book an appointment at the CK Birla Hospital for a comprehensive and compassionate approach to childbirth.
Yes. During the onset of pregnancy, the hormone progesterone increases in our body. This increases the metabolism as well, causing daytime drowsiness and fatigue. In case this also happens to be a subsequent pregnancy, then looking after your other child might also make you very tired and, hence sleepy.
With the next trimester, it is imperative that the body gets ample rest in order to be able to carry the excess weight of the baby around all day. So even if there is uninterrupted sleep at night, it is good if you take frequent naps to stay rested and energised at the same time.
Research suggests pregnant women who don’t end up getting enough sleep during pregnancy, develop a higher risk of developing complications like: Preeclampsia, or high blood pressure (hypertension). This means that there will be problems during the birthing process making it risky for both the mother and her child.
Pregnancy back pain gets worse at night because of the venous engorgement in the pelvis. As the uterus expands it presses on the vena cava, which is the main vein responsible for the circulation of blood from the heart onto the lower parts of the body, including feet. This happens particularly at night when the expectant mother is lying down.
To relieve this make sure that there is ample pillow support all around to keep the position comfortable for the mother without affecting the position of the baby. Apart from this
The world is moving at a break-neck speed and we are all trying to power our way through it. In the process, we are all compromising our health in some way or the other. With so much happening around us, our minds are overworked and tired, and so is the neck that holds it up.
Roughly 80% of the world’s total working population suffers from neck pain at one time or another. Out of which half the population consists of those suffering from chronic pain. There are multiple causes for this which range from wrong sleeping posture to osteoarthritis.
So what causes this pain in the neck? How can we prevent it? And what to do if the pain is unbearable? To know all about this and more, read on…
Table of Contents
When you experience pain in your neck muscles and it does not go away for a while then you are having neck pain. This is a common problem and poor posture is often responsible for this in most cases. But there can be various causes, but very rarely it is linked to any serious problem. In most cases, the cause of pain is rooted back to our everyday habits and movements.
Neck is a vital connective part of our body. It is responsible for supporting our head. So whenever the neck pains it somehow impacts the entire body since the movement of our body is restricted. So what are the possible causes of this pain, let us find out:
Apart from this, a recent study suggests that psychological risk factors also play a role in neck pain. Long-term stress, lack of social support, anxiety, and depression might trigger neck pain as well.
Source: https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-021-04957-4
Now that we know what can be the possible causes of neck pain, it is safe to say that the situation is not alarming in any way unless you are suffering from any pre-existing life-threatening disease.
It’s possible that our daily activities are causing our neck to hurt. Your neck is a complex blend of muscles, bones, ligaments, nerves, and tendons which hold your head in place. It is the pathway to your brain. It can become stiff or painful because of the posture and sleeping habits that put stress or strain on them.
The following are the main signs and symptoms associated with neck pain:
Experiencing neck pain due to bad posture can be managed by applying a warm compress on the neck to soothe the nerves and muscles. One can also get relief with over-the-counter balm or medications. However, if the pain is
Immediately seek medical help from your physician. It is seen that in most cases this pain is related to the spine. The more we lead a sedentary lifestyle the more the chances of pain tend to increase. So when seeking a physician it is advisable to seek consultation from a spine specialist.
The most prominent cause of neck pain is poor posture and age-related weakness of muscles and tissues. To help prevent this
At the CK Birla Hospital, Gurgaon we have a specialised wing of spine care specialists who are prepared to deal with any and every ailment related to the spine and spinal cord. With over 40 years of combined experience and some of the best specialists in Delhi NCR, we ensure every patient gets the best treatment and lasting relief. Set up an appointment with a doctor at Ck Birla Hospital.
It is a serious problem when
There are seven types of neck pains depending on the point of origin of the pain.
The ideal doctor would be orthopaedic since they would be able to assess the state of the muscles, tissues and bones. If the pain is isolated to the nerves, then it is a nerve disorder and needs the attention of a neurologist.
The ideal doctor would be a spine specialist since they would be able to assess the state of the muscles, tissues and bones. A spine specialist has specialised experience in handling the nerves and bones governing the spine and spinal cord. Based on their judgement and assessment they might refer the patient to a neurologist for nerve triggers or an orthopaedist for bone-related problems.
Congratulations! You have entered the third trimester of your pregnancy! It is amazing how you have been able to overcome some of the most testing phases of your pregnancy journey. Now, all we do is make sure we welcome the baby in the most healthy and happy way. Your pregnant belly is booming and you are glowing in anticipation with the happy pregnancy hormones doing their job.
This is also a time when you and your family start planning for the actual delivery. How to choose a birthing plan? How to remain agile during this phase? What are the best sleeping positions? How to ensure breastfeeding is properly done? For that here’s a brief guide on how to prep for your delivery.
But in the third trimester, what are the problems pregnant women need to deal with? What should you eat, what should you avoid, there are a whole lot of questions you need answers to. Don’t worry, just read on…
Table of Contents
Pregnancy happens in 3 stages of 3 months each called trimester. When you reach week 27 of your pregnancy tenure, it means you’re now in your third trimester. In an ideal scenario, this trimester ends at week 40, however, depending on your condition or complications it ends when your baby is delivered. A full-term pregnancy ranges between weeks 37 to 42 of pregnancy. Anything before week 37 is considered premature, and if your baby has not arrived by week 42, your OB-GYN will induce labour to avoid complications or opt for a c-section if there are complications.
Currently, around 49.4% of pregnancies in India are under the high-risk pregnancy bracket as per research data. This is why it is very important to be extra careful in the final trimester to avoid unwanted complications.
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10502764/
The third trimester is more tiring and uncomfortable than the other two trimesters primarily because the embryo grows to its full form. The discomfort is mainly attributed to the baby’s position and size, and with the due date approaching soon, anxiety also reaches its peak, making this trimester emotionally challenging as well. It is very important that at this stage you remain positive and try to adapt to the upcoming changes. Here is what you can expect during this stage:
It is essential that you take all sorts of health and medical precautions for some of the most commonly seen problems during the third trimester of pregnancy. These are:
Apart from this adequate prenatal care should be taken w.r.t. Your babies, such as checking the baby’s progress in terms of size, heart rate, position and movements. Make sure you and your gynaecologist have chalked out a proper birthing plan and made your choices.
During the third trimester, you will need frequent checkups, especially during week 32 to week 36. The doctors will check your weight and blood pressure and thoroughly examine you for any signs or symptoms you experience. Take your vaccines and more importantly the doses of tetanus, diphtheria and acellular pertussis (Tdap) vaccines. These are recommended for each pregnancy ideally taken between weeks 27 and 36 of the third trimester. This will build immunity for the baby at the time of birth.
There are ample emotional changes in expectant mothers. Some are good and some not so good, but it must be ensured that the mother is always in a positive frame of mind.
Make a checklist of all the things you will need during your third trimester. Start with charting out a birthing plan with your OB-GYN and healthcare provider. This will include monitoring your health pre-labour, any concerns that may indicate a c-section and consultations post-delivery.
At the CK Birla Hospital®, we take pride in planning things out for our expectant families for a seamless and memorable experience of welcoming a child into this world. For this, we don’t leave any stones unturned.
Everyone who sees you now is extra careful around you and more attentive to your needs. This is by far the second-best feeling during a pregnancy trumped only by the news of the baby’s arrival. But like they say, “with great power comes great responsibility”. This is why, our hands-on team of professional caregivers make sure you are well supported and looked after in a homely atmosphere, under compassionate care. Check out our comprehensive maternity package offer here (link to offer blog)
There is a virus ready to affect your body the moment your immunity shows the slightest dip. The onset of the recent pandemic has increased our general awareness about our health and possible diseases incredibly. One of the silent pandemics the world is still suffering from is cancer. This has been there for a long time mostly without a cure. Cervical cancer is also becoming a growing concern worldwide affecting a few men and mostly women. Its main cause is HPV or human papillomavirus.
What are the ways this virus attacks? Is it contagious? Is there any cure?
Table of Contents
The widely popular Human papillomavirus (HPV), can affect different parts of your body. There are over 100 types, including strains that cause warts on different parts of your body.
Roughly 30 HPV strains can affect your genitals, this includes your vulva, vagina, cervix, penis, scrotum, rectum and anus. Most of these are sexually transmitted infections (STIs) that pass on through skin-to-skin contact. However, the majority of genital HPV strains are harmless, including those responsible for genital warts. But others can be potentially high-risk variants, which may lead to cervical cancer. Early detection can lead to better results and prevent cancer from becoming severe. This leads us to the next question: Are all warts HPV?
Yes. All warts happen due to HPV, but all forms of HPV do not form warts. But whether or not these are fatal is the main concern. The HPV strains which lead to genital warts are nuisances.
The other types of HPV warts are:
| Flat Warts | smooth, flat-headed, fleshy or brownish-coloured bumps. |
| Plantar Warts | Small rough growths around the balls of the feet. |
| Common Warts | Small, grainy skin growths on your fingers or hands. These warts are transmitted by touch. |
| Periungual and Subungual Warts | These happen around your nails and fingers and disappear on their own. |
The type of HPV that can progress to cancer doesn’t cause warts. Which brings us to the next question: How is HPV related to cervical cancer?
HPV type 16 and type 18 can cause cervical dysplasia. Simply put this changes the cells of your cervix, the opening between your vagina and your uterus in women. When it is left untreated, it tends to advance to cervical cancer. Up to the age of 30, most HPV strains clear up by themselves. If found during a pap smear, it is advisable to perform regular screening to ensure the risk is eliminated at the onset. This then brings up the next question: Who is at a higher risk of getting HPV?
Irrespective of your reproductive anatomy, it’s vital to prevent HPV by either getting vaccinated and/or practising safe sex.
You Can Also Read: All you need to know about cervical cancer | Know your risk
First and foremost one must understand how one can get an HPV infection.
HPV is highly contagious since it spreads easily via skin-to-skin contact. No body fluids have to be exchanged either, so it will not spread through ejaculation (cum).
Genital HPV doesn’t usually come with any symptoms. The only visible symptom is a wart in your genital area. These are rough, cauliflower-like lumps that suddenly start growing on your skin. The timeline for the infection and the wart is not defined. It may appear weeks, months or even years after you’ve been infected. The only saving grace is that these are harmless.
The rest of the variants don’t have any symptoms. The only time the symptoms surface is when they progress to cancer. With cervical cancer, we must keep in mind that having HPV does not guarantee developing cancers.
The first step to any treatment is diagnosis. The doctor/ specialist will advise the following tests:
When the virus’s presence is confirmed, treatments will be prescribed. However, please note that once you get HPV it will never leave your body. So your healthcare partner will provide means to manage the situation by:
You Can Also Read: 10 Best Gynaecologists to Visit in Delhi-Gurgaon
Since the only way to prevent HPV is by abstaining from sex, here are some realistic ways in which you can protect yourself and your loved ones:
To conclude, HPV is a cause of concern but it can be prevented from escalating into cancer. As per WHO, the Human papillomavirus (HPV) is the name of a group of 200 known viruses, which can cause genital warts or cancer. Our body is able to control up to 90% of the existing HPV in our bodies, but a persistent infection can lead to Gynae, Uro and Cervical cancers. While HPV contributes to only 5% of all cancer cases worldwide, women are more likely to get it. Therefore a regular screening is essential.
Source: https://www.who.int/news-room/fact-sheets/detail/human-papilloma-virus-and-cancer
At the CK Birla Hospital, we understand the importance of being a reliable healthcare provider, especially in cases that need extra care. Our Gynae and Cancer specialists will not only help you prevent these morbid diseases but also guide you towards early detection, protection and treatment. Our judgement-free approach ensures we give the best possible treatment for your problem in the most compassionate and caring manner. To reach out to our sexual health experts book your appointment here.
Pregnancy is one of the most precious moments in a woman’s life. But it is also a time when women are most delicate, in terms of their bodies, mind and overall well-being. The main factor responsible for this is the changes that happen in her body, while the baby grows inside the womb. Additionally, some women also experience high blood pressure that might suddenly spike up if not monitored during pregnancy. This can put both the mother and her baby at risk during and after delivery.
High blood pressure or hypertensive disorders are preventable. But can these be prevented? Is there a way to properly manage the condition based on the stage of pregnancy? Yes. The good news is that it is both preventable and treatable.
Table of Contents
High blood pressure is a fairly common condition observed in most adults these days. Also called hypertension, it is observed among pregnant women between the ages of 20 to 44. However, when there is good control of blood pressure throughout the pregnancy, both the mother and her baby are likely to stay stable and healthy. This is why it is essential to get your medication sorted before, during and after pregnancy.
Monitoring high blood pressure is essential to avoid unwanted complications during pregnancy. This can impact both the mother and her baby.
Complications for the mother due to high BP:
Complications for the baby due to high BP:
| Pattern Delivery | The baby is born in less than 37 weeks of pregnancy. |
| Low Birth Weight | Baby weighs less than 5 pounds at birth |
| Malnourishment at birth | Lack of enough oxygen and nutrients in the womb causes this and triggers premature delivery. |
So given the extremity of the complications, if you are expecting or planning, you must discuss the problems with your healthcare partner before, during, and after pregnancy.
To understand the symptoms we need to understand the types of hypertensive disorders that might happen to a woman during her pregnancy.
The following profile of people are more likely to get preeclampsia:
You Can Also Read: A Guide to Increasing Baby Weight When 9 Months Pregnant
Depending on the stage of the pregnancy, the treatment approach will differ before, during and after pregnancy.
| Stage of pregnancy | Treatment and management of Hypertension |
| Before Pregnancy: When planning for pregnancy, set up a discussion with your healthcare partner or gynaecologist. | Make sure you discuss the following with your obstetrician:
|
| During Pregnancy | Once the pregnancy is confirmed, the following needs to be done in consultation with your Obstetrician:
|
| After Pregnancy | Once the baby is delivered monitor the following under the guidance of your doctor:
|
In conclusion, there can be multiple problems that can occur during a pregnancy, hypertension or high blood pressure is one of them. But this can be managed with proper planning and consultation with an experienced obstetrician. In case you are planning your pregnancy, it is always advisable to discuss your concerns with an expert who will give you the real picture based on your health. At the CK Birla Hospital, our expert OB GYNs provide holistic counselling and support to all our patients to prepare them physically and mentally towards a smooth pregnancy despite all concerns. Reach out to us to book an appointment.
With the flick of the wrist, a cricketer plays masterstrokes that make the team win matches. The same wrist is as work when you sweep and dust to keep your house clean. Our wrists do much more than just exist as a part of our bodies from where we can feel our pulse. Every time you want to know the time you look at your wrist, every time you hold something it involves your wrist. From typing to writing, cooking and even playing sports, our wrists make sure we are able to seamlessly move our hands to our needs. So when the wrists start to hurt, that’s when we realise exactly how much it contributes to a good quality of life for us.
So what can cause wrist pain? And what are the ways in which you can treat them?
Table of Contents
The wrist is a joint, connecting your hand and forearm. The wrist joint is made up of many small bones, which enable you to bend, straighten and rotate your hand. If you experience pain, numbness or tingling sensation in this region, then you are suffering from wrist pain. However, there is no need to be concerned about this pain as it is completely treatable. So now let us understand what are the reasons behind this pain in the next section.
As per the research carried out on risk factors associated with wrist pain by experts at the BMC Musculoskeletal Disorders, it was observed that women (14.7%) have a higher risk of getting wrist pain than men (5.6%). The study also indicated that those employed in manual labour and those who work out with weights are at a higher risk of getting wrist pain.
Source: https://d-nb.info/1206413336/34
Primarily any trauma impact on any part of the body will make it painful. So, if you have experienced a fall, and you have landed on your wrist, then it is bound to pain, due to the stress and trauma exposed to it. An X-ray will reveal whether this impact resulted in a sprain, fracture, or partial ligament disruption.

Otherwise, sometimes aches and pains may tend to appear out of the blue, with symptoms that may come and go. When the symptoms start getting worse or do not seem to subside for days then this will be termed chronic pain in the wrist. Get a healthcare provider to carefully examine the pain and obtain appropriate imaging studies to isolate the cause of the pain.
Some of the most identified causes of wrist pain are:
Depending on the cause of the pain the treatment approach will differ.
At home, you may do the following to help manage the pain:
If the orthopaedic identifies that the pain is chronic, then they might recommend
These days orthopaedic surgeons prefer using arthroscopic (minimally invasive) techniques to ensure a speedy recovery and complete treatment.
It is always said by medical practitioners that prevention is always better than cure. In the case of wrist pain, repetitive movements can tend to make it hurt more. For example, we all spend a lot of time typing. So you can avoid wrist pain from it by:
In conclusion, the underlying cause of pain once identified can help locate the cause and enable your healthcare partner to apply the appropriate treatment for it. When in doubt regarding pain that refuses to go away on its own, always reach out to a hand and wrist expert who will help resolve your problem. At the CK Birla Hospital, our award-winning team of experts and orthopaedic surgeons will provide the best solution with the fastest chance of recovery.
Table of Contents
The femur bone is the biggest and most significant bone in our body. It is found in our legs and it mainly connects the hip and the knee. A broken femur is therefore a serious injury that calls for immediate medical care. The only possible treatments are surgery and physical therapy. And these fractures are very painful, so a lot of pain medication is also prescribed.
Since the bone is the biggest and heaviest in our body, a femoral fracture often takes months to heal. Since the bone is big, the impact for fracture also has to be great. So one usually suffers from this during a car crash, an accident or an assault. Otherwise, elderly people who have weaker bones and are prone to injuries face this problem.
Since it is the biggest bone in your body, a femoral fracture will impact the quality of life of the person suffering from it. The possible consequences of a broken femur are:
When the injury happens it will show up the usual signs of pain, and swelling and in the worst cases the broken bone will pierce out of the skin of the leg. Rush to an orthopaedic, who will be able to physically examine the problem and suggest imaging tests to assess the extent of the injury.
Based on the results of X-rays and computed tomography scans (CT), the orthopaedic will diagnose the type of fracture and possible treatment options. The following types of fractures are usually diagnosed in a femoral fracture:
First and foremost the fracture must be cleaned and covered to avoid infection of any kind. Mostly, healthcare providers use a splint that will cover the whole leg. This splint goes up towards the hip. This is a temporary measure to help manage the pain, keep the bone in place and ensure the best outcomes.
Next, your healthcare provider will use traction to treat the fracture. These are broadly categorised into two types based on the placement of the traction:
If the fracture has happened, surgery will be performed within 24 to 48 hours to ensure the timely recovery of your injury. In this case, there are two types of surgical options available:
A fractured femur will mean that the internal skeletal framework of your leg has been compromised. So it will be extremely difficult to put any kind of weight or pressure on your leg. The bipedal movement of our legs needs the entire leg to function properly. So at any point, while walking we transfer our body weight on either of our legs to move. Since the fracture does not allow for any weight to be put on it, it will be very difficult to walk in this case. Support will be necessary for any kind of movement.
A fractured femur bone is an indication that the body will undergo a lot of pain and trauma due to the sheer magnitude of impact necessary to cause the break. The quality of life of the patient will be compromised and mobility will be substantially restricted. Since the events that lead to such painful and severe fractures are big, it will leave you with a long and tedious recovery tenure.
Even after the femur heals a significant amount of physiotherapy and rehab is required to reinstate the natural mobility of the person.
Recovery is very long for femoral fractures. It usually takes anywhere between 4 to 6 months. The length of your recovery also depends on the severity of your fracture, associated wounds and impact on the nerves and blood vessels around it. So even beyond the time when the trauma impact wears off, the pain sustains and involves a lot of pain medication to stabilise the condition. So the pain stays till the time the associated complications and the internal issues are completely healed.
A femoral neck fracture is a type of intracapsular hip fracture. This is because the femoral neck connects the femoral shaft with the femoral head. The femoral head connects with the acetabulum to form the hip joint. Therefore the conjunctional location of the bones makes the femoral neck prone to fracture. If the upper end of the femur bone has fracture this will therefore lead to a hip fracture, especially in patients with vitamin D and calcium deficiency.
अस्वस्थ जीवनशैली, गलत पान-पान, फ़ास्ट फूड्स, कोल्ड ड्रिंक्स, निष्क्रियता आदि हमारे जीवन का एक अहम् हिस्सा बन चुके हैं। इन सबकी वजह से हमें कई तरह के प्रॉब्लम्स का सामना करना पड़ता है जिसमें से एक है पित्त की पथरी। वैसे तो यह समस्या किसी भी उम्र के व्यक्ति को हो सकती है।
लेकिन अधिकतर मामलों में यह महिलाओं और अधिक उम्र के लोगों में देखने को मिलता है। पित्त की पथरी एक गंभीर समस्या है जिसका समय पर उचित निदान और उपचार कराना आवश्यक है, क्योंकि एक समय के बाद यह असहनीय दर्द, सूजन, संक्रमण और दुर्लभ मामलों में कैंसर का कारण भी बन सकता है।
पित्त की पथरी के दो प्रकार होते हैं जिसमें पहला कोलेस्ट्रॉल स्टोन और दूसरा पिगमेंट स्टोन है।
पित्त की पथरी होने पर कभी-कभी मरीज को कई महीनों या 1-2 सालों तक लक्षण अनुभव नहीं होते हैं। लेकिन जैसे-जैसे पथरी का आकार बढ़ता है, इसके कारण पित्ताशय में सूजन और दूसरी समस्याएं शुरू होती हैं – मरीज खुद में अनेक लक्षणों को अनुभव करना शुरू कर देते हैं।
पित्त की पथरी के मुख्य लक्षणों में निम्न शामिल हो सकते हैं:
इन सबके अलावा, आप अन्य लक्षण भी अनुभव कर सकते हैं। अगर आप ऊपर दिए गए लक्षणों को खुद में अनुभव करते हैं तो आपको बिना देरी किए विशेषज्ञ डॉक्टर से परामर्श करना चाहिए। आमतौर पर डॉक्टर पित्त की पथरी का निदान करने के बाद उपचार की प्रक्रिया शुरू करते हैं।
पित्त की पथरी का निदान करने के लिए डॉक्टर सबसे पहले मरीज से उनके लक्षणों के बारे में कुछ प्रश्न पूछते हैं, मरीज का शारीरिक परीक्षण करते हैं और फिर कुछ विशेष जांच करने का सुझाव देते हैं। पित्त की पथरी का निदान करने के लिए निम्न जांच किए जाते हैं:
इस जांच के दौरान, डॉक्टर मरीज का ब्लड सैम्पल लेकर उसे लैब में जांच करने के लिए भेजते हैं। खून जांच के दौरान, पित्त की पथरी के कारण संक्रमण, पीलिया, अग्नाशयशोध (पैंक्रियाटाइटिस) या दूसरी जटिलताओं के बारे में पता लगाया जाता है।
इस दौरान, डॉक्टर पित्त की पथरी की तस्वीर प्राप्त करते हैं जिनकी मदद से पित्ताशय के मोटापा और सूजन की पुष्टि करने में मदद मिलती है।
जब अल्ट्रासाउंड के दौरान छोटी पथरी की पुष्टि नहीं हो पाती है तो उसके बारे में पता लगाने के लिए डॉक्टर एंडोस्कोपिक अल्ट्रासाउंड का सुझाव देते हैं। इस जाँच के दौरान, डॉक्टर एंडोस्कोप नामक उपकरण का इस्तेमाल करके छोटी आकार की पथरी को आसानी से देख पाते हैं।
इमेजिंग परीक्षण के दौरान डॉक्टर सिटी स्कैन, ओरल कोलेसिस्टोग्राफी, हेपेटोबिलरी एमिनो डायसोटिक एसिड स्कैन, मैग्नेटिक रेजोनेंस कोलेजनोपैंटोग्राफी या एंडोस्कोपिक रेट्रोग्रेड कोलेजनोपैनोग्राफी आदि जांच प्रक्रियाएं करते हैं।
आवश्यकता होने पर, ऊपर दिए गए जांचों के आलावा डॉक्टर अन्य भी जांच करने का सुझाव दे सकते हैं। सभी जांचों के परिणामों के आधार पर डॉक्टर उपचार करते हैं। पित्त की पथरी के उपचार में घरेलू नुस्खे, आयुर्वेदिक जड़ी-बूटियां, होम्योपैथिक दवाएं, एलोपैथिक दवाएं और सर्जरी आदि शामिल हैं।
सर्जरी ही पित्त की पथरी का एकमात्र सफल और परमानेंट इलाज है। उपचार के दूसरे माध्यमों से पित्त की पथरी के लक्षणों को कम किया जा सकता है। अगर आप खुद में पित्त की पथरी के लक्षणों को अनुभव करते है या इससे पीड़ित हैं तो हमारे डॉक्टर के साथ परामर्श कर उचित उपचार प्राप्त कर सकते हैं।
प्रश्न 1. क्या पित्ताशय की पथरी अपने आप घूल सकती है?
पित्त पथरी अपने आप दूर हो सकती है, लेकिन आमतौर पर ऐसा नहीं होता है और उपचार की आवश्यकता हो सकती है। पित्ताशय की पथरी हमेशा लक्षणों का कारण नहीं बन सकती है, और उन मामलों में, जटिलताओं को रोकने के लिए केवल आहार परिवर्तन ही आवश्यक हो सकते हैं। लोग पित्ताशय की थैली के बिना सामान्य जीवन जी सकते हैं।
प्रश्न 2. पित्त की पथरी के क्या कारण हैं?
पित्ताशय में पथरी बनने के अनेक कारण होते हैं। इसमें मुख्य रूप से अस्वस्थ जीवनशैली, गलत खान-पान, मोटापा, कम मात्रा में पानी पीना, तेजी से अजान कम करना, जंक फूड्स और कोल्ड ड्रिंक्स आदि का सेवन आदि।